Pre-exposure prophylaxis (PrEP) is a preventive healthcare strategy shown to reduce HIV incidences significantly. By taking PrEP, individuals at high risk of HIV can decrease their chances of infection through its effective mechanisms as approved by global health organizations. This article explores PrEP's workings and its role in public health.
Pre-exposure prophylaxis, commonly known as PrEP, is a medical practice that has revolutionized the prevention of HIV. With HIV being a persistent epidemic around the world, PrEP offers a beacon of hope through its capacity to significantly lower the risk of infection in high-risk groups. Since its approval by health organizations like the CDC and the World Health Organization, PrEP has gradually integrated into public health strategies aimed at controlling and eventually eradicating the spread of HIV.
The impact of PrEP is especially notable in urban areas and among populations disproportionately affected by HIV. Increased awareness and accessibility have led to greater adoption of this preventive measure, contributing to declines in new infections in many parts of the world. For many, understanding what PrEP is, how it works, and who can benefit from it is pivotal not only for personal health but also for community health at large.
PrEP involves the regular intake of a specific antiviral medication. Typically, it comprises tenofovir and emtricitabine, which hinder the virus's ability to replicate within the body. For PrEP to be effective, consistent and timely consumption of the medication is crucial. According to clinical studies, daily adherence to PrEP results in more than 90% effectiveness in preventing HIV transmission through sexual contact and is about 70% effective for injection drug users when combined with behavioral interventions.
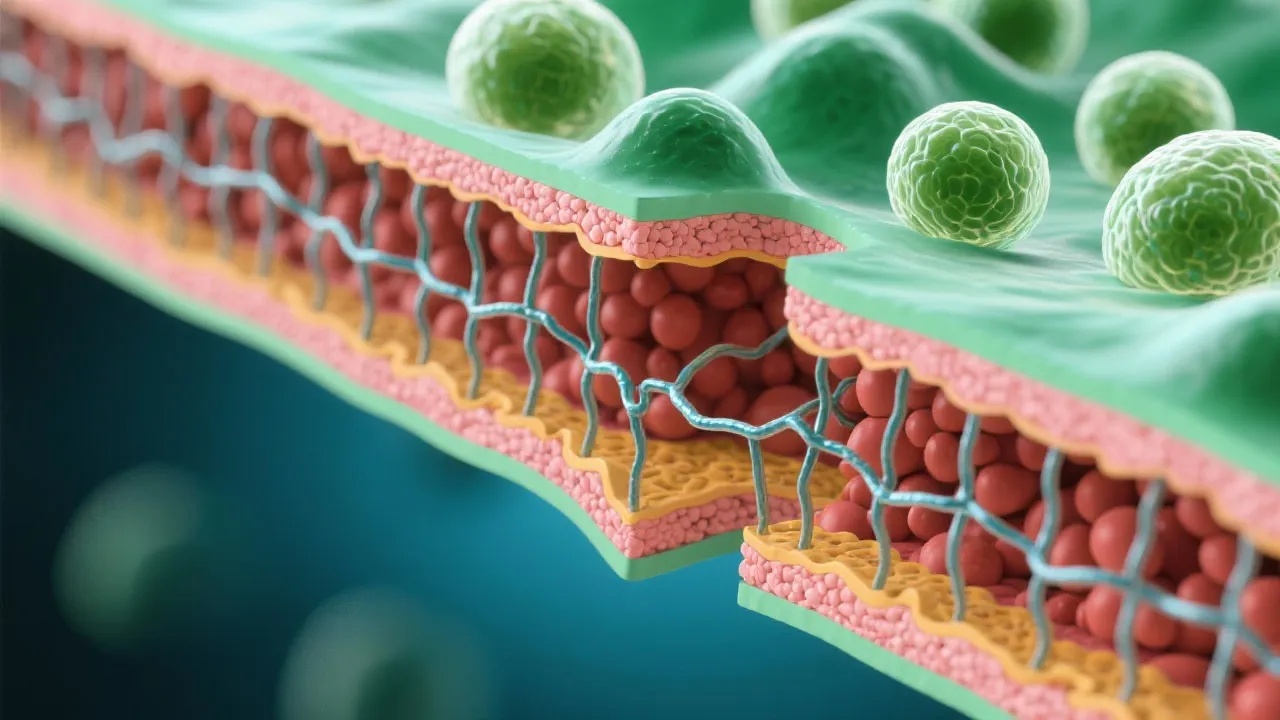
To comprehend how PrEP functions on a biological level, it is essential to delve into the mechanisms of the medications used. Tenofovir is a nucleotide analog that disrupts the viral replication process by hindering the reverse transcriptase enzyme essential for HIV's replication. Emtricitabine works similarly, further inhibiting the virus's ability to multiply. When taken consistently as prescribed, these medications significantly reduce the possibility of HIV establishing an infection, even if the virus is present in bodily fluids during potential exposure moments.
Moreover, health organizations have emphasized the importance of education surrounding PrEP. This includes ensuring users understand the necessity of adherence to the medication regimen, the potential side effects, and the need for regular follow-ups. These steps not only enhance the effectiveness of the medication but also empower users with knowledge about their sexual health and HIV prevention.
PrEP is recommended for individuals at substantial risk of contracting HIV, including men who have sex with men, heterosexual men and women with an HIV-positive partner, and those who share needles. Recent data suggests that when properly implemented, PrEP usage can lead to a noteworthy decline in the incidence of new HIV cases, thus proving its utility in global health frameworks aimed at halting the spread of the virus.
Identifying and reaching out to target populations is crucial for effective PrEP implementation. Efforts to promote PrEP must address specific demographics that face higher HIV risks, such as young men of color, individuals in serodiscordant relationships, and transgender people. Tailoring outreach efforts to speak to the unique challenges these groups face—such as stigma, discrimination, and barriers to healthcare access—can significantly increase PrEP uptake. Public health campaigns that are inclusive and culturally competent may foster a more comprehensive approach to HIV prevention.
Additionally, community organizations that serve high-risk groups can play an instrumental role in providing education about PrEP. Through workshops, informational sessions, and one-on-one consultations, these organizations help demystify PrEP and promote its availability and benefits, encouraging individuals to seek this preventive measure. Collaborative networks between healthcare providers and community organizations enhance outreach to those in need.
The primary benefit of PrEP is its preventive capacity, which empowers individuals to take control of their health, especially in circumstances where exposure risk is high. Additionally, PrEP is part of an integrated approach to sexual health, often combined with the use of condoms, regular STI checks, and educational programs. However, considerations need to be made regarding potential side effects, such as kidney function impairment, and the importance of regular medical consultations to monitor health conditions.
In essence, the emotional and psychological benefits of using PrEP can also not be overlooked. For many, taking an active step toward prevention can greatly reduce anxiety regarding HIV, allowing individuals to engage in their sexual lives with greater confidence. This mental health aspect is vital, as anxiety about potential HIV exposure can lead to decreased quality of life for many at risk.
However, while PrEP presents a highly effective preventive strategy, it is essential that individuals remain vigilant about the other facets of their sexual health. PrEP does not protect against other sexually transmitted infections (STIs) or unwanted pregnancies, and thus should be considered a part of a larger risk-reduction strategy. Emphasizing the complementarity of using condoms and conducting regular testing can optimize sexual health outcomes for individuals relying on PrEP.
Access to regular follow-up care and the opportunity to discuss any side effects or concerns with healthcare professionals is a fundamental aspect of the PrEP experience. Patients benefit from consistent monitoring not only to ensure the ongoing effectiveness of the medication but to facilitate educational dialogues about safe sexual practices and other health behaviors that can further reduce risk.
While these steps provide a clear pathway to accessing PrEP, the experience of obtaining PrEP can vary widely depending on individual circumstances and healthcare systems. Awareness of potential obstacles is crucial for prospective users. For instance, some individuals may face financial barriers, lack of insurance, or logistical issues regarding access to healthcare facilities. Understanding these potential challenges is the first step toward addressing them.
Community-based organizations and non-profits may offer vital resources to help navigate barriers to accessing PrEP, including funding assistance, transportation services, and peer support groups. By leveraging these resources, individuals can overcome challenges that might impede their ability to obtain or continue using PrEP. The role of community health workers is particularly important in providing personalized support and facilitating connections to necessary healthcare services.
In the broader context of public health, PrEP is not only a preventive tool; it represents a strategic approach to curbing the HIV epidemic at local, national, and global levels. Integrating PrEP into public health initiatives has proven beneficial in mitigating the spread of HIV, especially in areas with high rates of infection. Public health campaigns have engaged with substantial resources to ensure that vulnerable populations receive proper education and access to PrEP.
The concept of treatment as prevention (TasP) complements PrEP initiatives as well. Encouraging individuals already diagnosed with HIV to engage in antiretroviral therapy to maintain an undetectable viral load not only benefits their health but also serves to reduce the risk of transmitting the virus to HIV-negative individuals. Together, PrEP and TasP create a dual-layered protective paradigm, reinforcing the message that HIV is manageable with proper healthcare access and education.
As health departments advocate for combined prevention strategies, the reduction in new HIV infections can be seen as part of larger initiatives to foster overall health equity in the populations most affected by HIV. Implementing outreach efforts that address social determinants of health—such as housing stability, economic opportunity, and education—can create a supportive environment for those most at risk of HIV exposure. Partnerships among healthcare providers, public health officials, policymakers, and community organizations are vital for creating a robust educational infrastructure.
| Question | Answer |
|---|---|
| Who should consider PrEP? | Individuals at high risk of HIV exposure, including those with HIV-positive partners, multiple partners, or injection drug users. |
| Is PrEP a vaccination? | No, PrEP is an oral medication taken regularly to prevent HIV infection, not a vaccine. |
| Can PrEP cure HIV? | No, PrEP is only a preventive measure. It cannot cure those already infected with HIV. |
| Are there side effects? | Very few users experience mild side effects, but severe side effects are rare. Regular check-ups are advised. |
| How effective is PrEP? | When taken correctly, PrEP can reduce the risk of getting HIV from sex by more than 90% and by about 70% for injection drug users. |
| How long does it take for PrEP to work? | PrEP becomes effective within 7 days for anal sex and 21 days for receptive vaginal sex, provided it is taken consistently. |
| Is PrEP covered by insurance? | Many insurance plans cover PrEP; however, coverage may vary, so checking with your insurance provider is recommended. |
PrEP represents a significant advancement in reducing HIV incidences worldwide. While offering substantial protection to those at heightened risk, it remains a key element within a more comprehensive strategy of risk reduction that includes education, regular testing, and behavioral changes. As awareness and access to PrEP expand, it is expected to play a pivotal role in the ongoing battle against HIV/AIDS, complemented by ongoing research and community engagement.
Understanding PrEP's potential to safeguard individuals against HIV empowers communities to take proactive steps toward their health. The engagement of various stakeholders, including healthcare providers, community organizations, and individuals, is essential for maximizing the adoption and effectiveness of PrEP. Continued public discussion around HIV prevention methods—though vital—must also evolve beyond PrEP to encompass a holistic view of sexual health that considers emotional, physical, and social well-being.
In conclusion, as we move forward into a future where HIV is not only manageable but preventable, PrEP must be seen as a cornerstone in the fight against this virus. Its successful deployment across diverse populations—and the ensuing partnerships that arise from it—will remain crucial in shaping a world where HIV does not dictate lives or dominate conversations around health and sexuality. The vision for an HIV-free future is attainable, and with combined efforts, renewed commitment, and advocacy, we can work toward achieving this imperative global health objective.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
