NAFLD-related HCC is an emerging concern in liver disease. As a significant health issue, hepatocellular carcinoma (HCC) associated with nonalcoholic fatty liver disease (NAFLD) is driving global research efforts. This article explores the link between these conditions, advancements in diagnosis, and emerging treatments, providing a comprehensive guide derived from expert insights on this rapidly evolving topic.
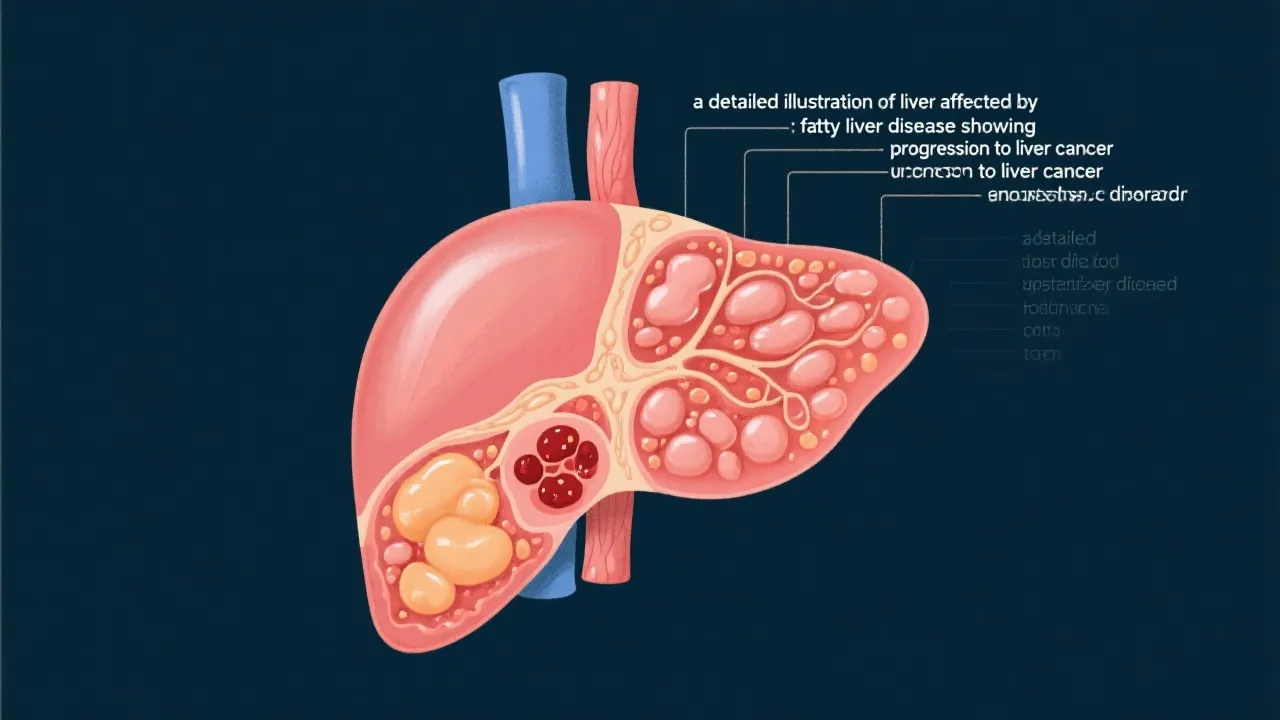
Nonalcoholic fatty liver disease (NAFLD) is increasingly recognized as a significant health concern worldwide due to its potential progression to hepatocellular carcinoma (HCC), commonly known as liver cancer. Hepatologists reveal that while NAFLD is primarily marked by excessive fat accumulation in the liver, its very severe complication is the development of HCC. Understanding this link is crucial for developing effective strategies to manage and treat the condition. Moreover, the global prevalence of obesity and type 2 diabetes, which are significant risk factors for NAFLD, underscores the urgency of addressing this public health challenge.
NAFLD-related HCC has become a topic of interest among researchers and healthcare professionals. The liver's vulnerability to fat accumulation can lead to inflammation, fibrosis, cirrhosis, and eventually cancer. While traditional risk factors for liver cancer include chronic hepatitis infection and alcohol abuse, NAFLD is now recognized as a major risk angle, especially in Western countries. This shift is not merely an epidemiological observation; it is also reflected in changing patterns of liver cancer incidences, which show a marked increase associated with rising rates of obesity and sedentary lifestyles. Researchers are working diligently to elucidate the biological and molecular mechanisms linking these two conditions.
The exact mechanism by which NAFLD progresses to HCC is complex and multifaceted. Genetic predisposition, lifestyle choices, and other metabolic comorbidities such as obesity and type 2 diabetes contribute significantly to this progression. A key element in this relationship is the development of nonalcoholic steatohepatitis (NASH), a more severe form of NAFLD characterized by inflammation and liver cell damage. Current studies suggest that molecular changes in liver tissue, induced by lipid metabolic disturbances, play a key role in carcinogenesis.
In particular, the accumulation of toxic lipids and inflammatory cytokines can provoke oxidative stress, leading to DNA damage and genomic instability, which are critical factors in the development of cancer. Moreover, insulin resistance, often associated with obesity and metabolic syndrome, plays a significant role in this pathway, augmenting hepatic fibrosis and the likelihood of malignancy. Other factors, such as aging and certain genetic mutations (like those affecting the PNPLA3 gene), can further exacerbate the risk of HCC among individuals with NAFLD.
Early diagnosis of NAFLD-related HCC greatly improves the prognosis for patients. Regular monitoring of individuals with NAFLD through imaging studies like ultrasound and MRIs, alongside serum biomarkers, is recommended. The identification of elevated liver enzymes—specifically alanine aminotransferase (ALT) and aspartate aminotransferase (AST)—can serve as an important initial indicator of liver dysfunction. However, diagnosis at very advanced stages occurs due to a lack of overt symptoms in earlier stages. Symptoms, when they do arise, might include unexplained weight loss, loss of appetite, or abdominal pain, all of which can often be mistaken for other health conditions.
In light of the silent progression of NAFLD, researchers are increasingly advocating for the implementation of screening recommendations for individuals at high risk—those with obesity, diabetes, and metabolic syndrome—allowing for early intervention before the onset of HCC.
The medical community is evolving its diagnostic toolkit to better detect early signs of liver carcinogenesis. Technologies such as elastography and FibroScan® have shown promise in assessing liver stiffness, which correlates with fibrosis and, consequently, cancer risk. Non-invasive methods, including serum biomarkers, are also being developed to identify individuals with NAFLD at higher risk of progression to HCC. Moreover, the emergence of liquid biopsies presents an intriguing frontier in oncology; they allow for the identification of cancer-related genetic alterations in circulating tumor DNA, providing insights into the tumor's characteristics without the need for invasive tissue sampling.
Artificial intelligence (AI) is becoming a crucial player as well in the diagnostic realm. Algorithms can help analyze complex datasets, enhancing the accuracy of predictions regarding disease progression based on nuanced patient data. Furthermore, machine learning techniques can identify patterns in imaging studies that may be difficult for the human eye to see. As these technologies continue to evolve, they hold the potential to significantly improve the accuracy and timeliness of HCC diagnoses, ultimately benefiting patient outcomes.
Once diagnosed, treatment of NAFLD-related HCC involves a multifaceted approach. Surgical resection, liver transplantation, and local ablative therapies, such as radiofrequency ablation and microwave ablation, are viable options depending on the stage of cancer. However, not all patients are appropriate candidates for surgery due to advanced age or underlying comorbidity.
Novel pharmaceuticals targeting the metabolic pathways involved in NAFLD are being actively researched. For example, drugs that improve insulin sensitivity or alter lipid metabolism are under investigation for their potential to reduce liver fat and, subsequently, the risk of cancer. Immunotherapy, which empowers the immune system to fight cancer cells, represents a promising frontier in treating this malignancy. Agents such as immune checkpoint inhibitors are being evaluated in clinical trials, showing potential in enhancing the body’s immune response against tumor cells in HCC patients.
Moreover, combination therapies that integrate conventional approaches with emerging modalities may yield better outcomes. Integrating strategies that target different aspects of the disease could represent the best therapeutic route forward, providing a more tailored treatment for patients based on their unique cancer profiles.
Prevention remains key in combating NAFLD-related HCC. Lifestyle modifications such as adopting a balanced diet, regular physical activity, and maintaining a healthy weight are fundamental. A diet low in saturated fats and rich in fruits, vegetables, and whole grains has been shown to support liver health. Evidence suggests that the Mediterranean diet, which emphasizes healthy fats and lean proteins, may be particularly beneficial in preventing NAFLD progression.
Regular exercise has been widely recommended, not only for weight management but also for its ability to improve insulin sensitivity and reduce liver fat. Even moderate-intensity exercise, such as brisk walking or cycling, can have profound impacts on liver health. These steps help mitigate risk factors and prevent the progression of NAFLD to HCC. Healthcare providers stress education as a vital tool in both prevention and early detection efforts. Public health campaigns highlighting the risks associated with NAFLD and the importance of routine screening can play a pivotal role in increasing awareness and preventing the disease's progression.
Additionally, promoting initiatives within communities that encourage healthy eating and active lifestyles can create a supportive environment conducive to making sustainable health choices. Involving schools, workplaces, and local organizations in these initiatives can further reinforce healthier habits across the population.
Dr. Alisha Kumar, a leading hepatologist, asserts that interdisciplinarity in research and treatment is essential for tackling NAFLD-related HCC. "Bridging gaps between metabolic research, oncology, and hepatology could potentially reshape our approach to this challenge," she emphasizes. This multidisciplinary approach not only enhances our understanding of disease mechanisms but also fosters collaboration among various healthcare professionals to provide comprehensive patient care.
Furthermore, the integration of AI in predicting individual risk is posited as a future direction that holds much promise. AI-driven platforms can assist in developing personalized treatment plans, assessing patient risk profiles, and evaluating treatment responses. These advancements will likely lead to more precise and effective management strategies tailored to the unique characteristics of each patient.
Additionally, ongoing dialogues among researchers, clinicians, and public health officials are critical to disseminate the latest findings and interventions. Engaging in forums and scientific conferences can facilitate the sharing of knowledge, driving forward advancements in understanding the relationship between NAFLD and HCC.
NAFLD is a condition characterized by excess fat storage in liver cells not caused by alcohol consumption. It encompasses a spectrum that ranges from simple steatosis to more severe inflammation and fibrosis.
Over time, NAFLD can cause inflammation and damage to liver tissues, leading to cirrhosis and increasing the risk of liver cancer. The progression typically involves the transition from NAFLD to NASH, which heightens the risk of liver cell malignancy.
Yes, with lifestyle changes including dietary modifications and regular exercise, NAFLD can often be reversed, particularly if caught early. Many patients experience significant improvements in liver health following lifestyle interventions.
Treatment options include surgery, liver transplantation, ablation therapies, and novel drugs targeting metabolic pathways. The choice of treatment is contingent on the cancer stage, the patient's overall health, and specific tumor characteristics.
NAFLD-related HCC presents significant challenges due to its silent progression and late diagnosis. Advances in medical technology and research into the metabolic underpinnings of liver carcinogenesis afford new hope in the prevention and treatment of this condition. Emphasizing prevention through lifestyle alterations and early detection could drastically alter the landscape of liver cancer treatment and outcome. Increased awareness, community engagement, and interdisciplinary collaboration represent key strategies for tackling this growing health issue. As research continues to elucidate the mechanisms underlying NAFLD and its progression to cancer, healthcare systems must adapt, ensuring patients receive optimal care while also focusing on prevention strategies to mitigate the escalating burden of liver disease.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
