This article explores the intricate relationship between Non-Alcoholic Fatty Liver Disease (NAFLD) and Hepatocellular Carcinoma (HCC), two interconnected liver conditions that are increasingly prevalent. NAFLD is characterized by excess fat buildup in the liver, which can progress to HCC, a primary form of liver cancer. Understanding their connection is essential for early detection and management strategies.
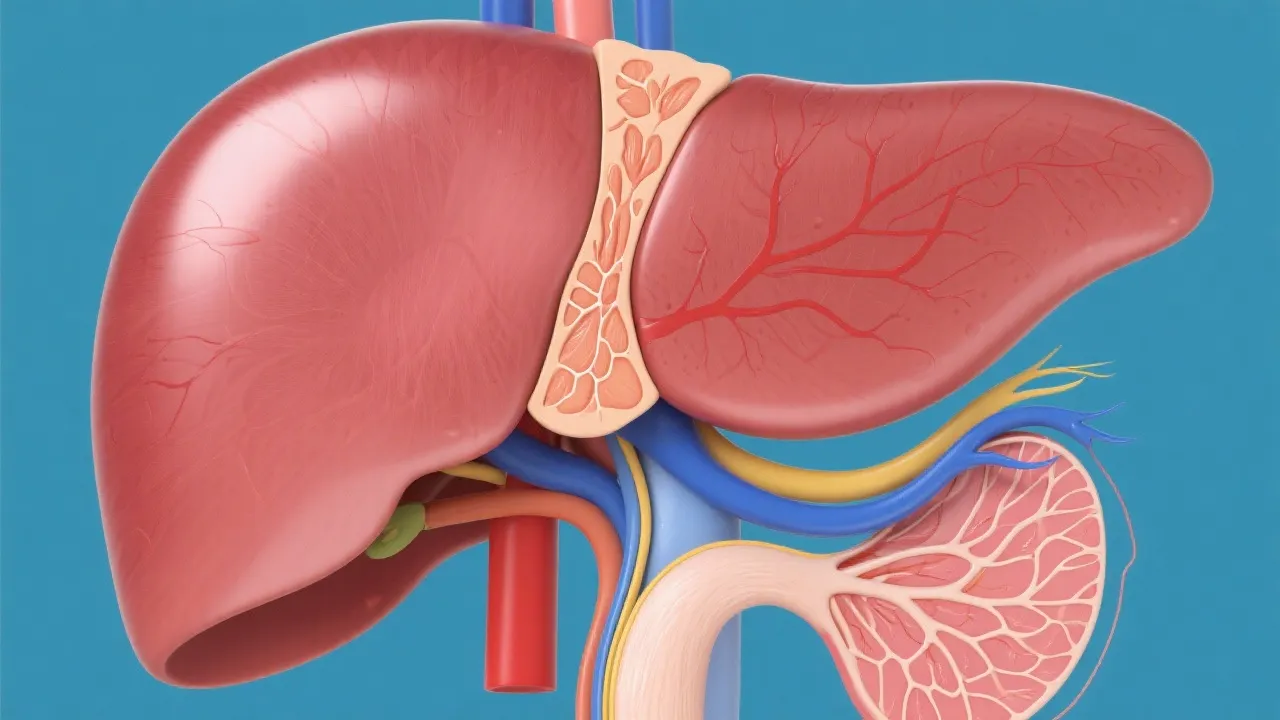
A growing body of research indicates a strong connection between Non-Alcoholic Fatty Liver Disease (NAFLD) and Hepatocellular Carcinoma (HCC). NAFLD is recognized as the accumulation of excess fat in liver cells in individuals who consume little or no alcohol. Furthermore, prevalence rates have surged in recent years, making NAFLD one of the most common liver disorders in the world. It is estimated that about 25-30% of the global population is affected by NAFLD. Over time, NAFLD can progress to non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis, and potentially HCC, a primary form of liver cancer. The link between NAFLD and HCC is concerning due to the escalating rates of obesity and metabolic syndrome globally. Understanding this progression is vital for implementing effective prevention and treatment strategies to mitigate the risk of liver cancer.
NAFLD is caused by a variety of factors, including obesity, insulin resistance, metabolic syndrome, and genetic predispositions. The condition is diagnosed when more than 5% of hepatocytes showcase steatosis without significant alcohol use. The accumulation of fat in liver cells triggers a series of pathological processes, including oxidative stress, lipotoxicity, and inflammation. Initially, the process begins with simple steatosis, which can progress to NASH if left unmanaged. NASH, characterized by inflammation and liver cell damage, significantly increases the risk of progressing to cirrhosis and eventually HCC. The interplay between these processes is complex: inflammation further exacerbates insulin resistance, creating a vicious cycle that accelerates disease progression.
Moreover, certain genetic variants have been identified that increase susceptibility to NAFLD and its progression. For instance, variants in the PNPLA3 gene have been associated with increased liver fat levels and a higher risk of progression to NASH and fibrosis. Additionally, the gut microbiome has gained attention as a possible contributing factor, with alterations in the composition of gut bacteria being implicated in the pathogenesis of NAFLD and NASH.
The progression from NAFLD to HCC is complex and multifaceted. Chronic inflammation and cell death in NASH create an environment conducive to cancer development. DNA damage, cellular turnover, and regenerative proliferation further contribute to this transformation. As cirrhosis sets in, the risk of developing HCC grows exponentially due to the sustained state of liver cell damage. Studies indicate that the development of HCC often occurs in the backdrop of cirrhotic liver disease, when the liver architecture is significantly altered. This creates an environment ripe for malignant transformation, characterized by the emergence of dysplastic nodules and subsequent fast-growing tumors.
Furthermore, inflammatory cytokines and growth factors released during liver injury can promote tumorigenesis. For instance, increased levels of interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha) can result in increased hepatic cell proliferation and apoptosis, creating a microenvironment that favors the evolution of liver cancer. Understanding how these molecular mechanisms influence HCC development is crucial for advancing preventive and therapeutic measures.
Several risk factors increase the likelihood of NAFLD progressing to HCC, including age, male gender, genetic predispositions, and comorbidities such as diabetes and obesity. The diagnosis of HCC in patients with NAFLD often involves a combination of imaging techniques such as ultrasound, CT, or MRI, alongside serum biomarkers like alpha-fetoprotein (AFP). Elevated AFP levels can indicate tumor activity, but it is essential to note that not all HCC cases will have significantly elevated AFP, which restricts its utility as a standalone diagnostic tool.
In addition to imaging and tumor markers, newer technologies such as elastography and enhanced imaging techniques are being increasingly utilized to help diagnose liver diseases and assess the risk of HCC. Elastography assesses liver stiffness, which correlates with fibrosis and overall liver disease severity. Meanwhile, advanced imaging modalities, such as contrast-enhanced ultrasound or magnetic resonance imaging, are showing promise in signaling early-stage tumors not detectable by traditional imaging.
| Feature | NAFLD | HCC |
|---|---|---|
| Cause | Metabolic dysfunction | Chronic liver damage |
| Symptoms | Often asymptomatic | Jaundice, weight loss, abdominal pain |
| Diagnosis | Imaging and biopsy | Tumor markers and imaging |
| Treatment | Lifestyle changes, medications | Surgical, systemic therapies |
Preventing progression from NAFLD to HCC involves managing underlying risk factors. This includes adopting a healthy diet, maintaining physical activity, and managing metabolic conditions like diabetes and hypertension. Weight loss is particularly crucial for patients with NAFLD; even a modest reduction in weight can significantly improve liver histology and may reduce the risk of liver cancer. Several guidelines advocate for dietary patterns rich in unsaturated fats, such as the Mediterranean diet, to combat the progression of NAFLD.
Moreover, there has been an increasing focus on the role of pharmacotherapy in managing NASH. Emerging treatment options like SGLT2 inhibitors and GLP-1 receptor agonists for diabetic patients have shown potential benefits in alleviating hepatic steatosis and inflammation related to NAFLD. Current clinical trials are investigating new agents, including novel anti-fibrotic medications and metabolic modulators, extending hopes for effective NAFLD treatment.
For advanced cases, therapeutic approaches may include medications such as pioglitazone and vitamin E for NASH, while HCC management may involve surgical interventions, liver transplantation, and systemic therapies. For patients diagnosed with HCC, treatment strategies typically depend on the tumor stage. Early-stage HCC can often be addressed with resection or ablation techniques, whereas advanced cases may require systemic therapies such as immune checkpoint inhibitors and targeted therapies, which are being evaluated in clinical trials.
What is the primary cause of NAFLD? NAFLD is primarily caused by obesity, insulin resistance, and metabolic syndrome. Additionally, certain genetic and environmental factors further predispose individuals to develop this condition.
Can NAFLD lead directly to liver cancer? While NAFLD itself does not cause cancer, its progression to NASH and cirrhosis significantly increases the risk of HCC. The chronic inflammation associated with NASH plays a pivotal role in initiating oncogenic processes in the liver.
What is the very reliable method to screen for HCC in chronic liver conditions? Regular imaging tests like ultrasound combined with liver function tests and tumor markers are recommended for HCC screening in high-risk patients, particularly those with cirrhosis or advanced fibrosis.
Is liver biopsy necessary for diagnosing NAFLD or HCC? A liver biopsy is the gold standard for diagnosing NAFLD progression but is not typically required for initial evaluations. HCC diagnosis primarily relies on imaging and AFP levels, supplemented by the patient’s clinical history.
What lifestyle changes can mitigate the risk of NAFLD? Adopting a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, combined with a regular exercise routine and weight management, are critical in reducing NAFLD risk. Limiting alcohol intake and avoiding other hepatotoxic substances are also recommended.
Living with NAFLD can be challenging for patients as they navigate the uncertainties associated with the condition. Many patients feel overwhelmed by their diagnosis, especially knowing that it can potentially lead to more severe health issues, such as liver cancer. Psychological support and patient education play essential roles in managing anxiety and improving overall well-being. Patients often benefit from attending support groups where they can share experiences and coping strategies with others facing similar challenges. This communal support not only provides emotional solace but also encourages adherence to lifestyle changes that are crucial for managing NAFLD.
Additionally, healthcare providers are crucial in providing patients with guidance tailored to their individual circumstances. Personalized management plans that include nutrition counseling, physical activity recommendations, and regular follow-ups are vital in helping patients engage in their health care more proactively. Encouraging patients to track their progress can also be motivating, as seeing incremental improvements can reinforce positive behavior changes.
Continuous research into NAFLD and its progression to HCC is vital for improving patient outcomes and understanding the underlying mechanisms of disease. Novel insights into the biology of NAFLD have opened doors to potential therapeutic avenues, illustrating the necessity of ongoing clinical trials. Research institutions and universities worldwide are studying various aspects of NAFLD, from genetic factors and dietary influences to pharmacological interventions, which may pave the way for groundbreaking treatments.
Moreover, interdisciplinary approaches that integrate insights from epidemiology, genetics, and molecular medicine could provide comprehensive strategies to combat NAFLD. Collaborative efforts among researchers, clinicians, and healthcare organizations are essential to create evidence-based guidelines and promote awareness among healthcare professionals and the general population regarding the importance of early detection and intervention.
NAFLD and HCC are not just regional problems; they are global health challenges that require a concerted international response. Different countries experience varying prevalence rates and approaches to managing these diseases due to cultural, economic, and healthcare system differences. In countries with high obesity rates, such as the United States, NAFLD is becoming an urgent public health issue. Conversely, in low- to middle-income countries, the rapid adoption of Western lifestyles and dietary habits is leading to a surge in NAFLD cases among previously unaffected populations.
International organizations, including the World Health Organization (WHO), are recognizing NAFLD as a growing health burden and are encouraging countries to take action against metabolic diseases. Policy measures aimed at promoting healthier lifestyle choices, educating the public on the risks of obesity, and ensuring better access to healthcare can contribute significantly to reducing the incidence of liver diseases worldwide.
Understanding the link between NAFLD and HCC is critical in the realm of liver diseases. With lifestyle diseases on the rise globally, the incidence of these liver conditions also sees a concerning uptick. Through informed decision-making and early interventions, the transition from benign liver conditions to malignancies like HCC can be effectively curbed. Public health initiatives emphasizing education about nutrition and physical activity can lower the rates of obesity and metabolic syndrome, thereby reducing the burden of NAFLD. Continuous research and innovations in treatment pathways hold promise for altering the natural progression of these diseases, paving the way for improved patient outcomes. The collaboration between patients, healthcare providers, and researchers is essential to foster a comprehensive approach to tackle this pressing health issue, ultimately aiming for a future where liver cancer related to NAFLD can be averted or effectively managed.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
