Non-alcoholic fatty liver disease (NAFLD) linked hepatocellular carcinoma (HCC) is a significant cause of liver cancer worldwide. Highlighting the increasing prevalence of NAFLD as a precursor to HCC, this article delves into the complex relationships between these conditions, their implications, and the preventative measures being considered by experts in the field.
Understanding the progression from non-alcoholic fatty liver disease (NAFLD) to hepatocellular carcinoma (HCC) is crucial in managing and preventing liver cancer incidences effectively. As NAFLD becomes more prevalent, particularly in developed nations due to sedentary lifestyles and poor dietary choices, the incidence of related HCC has been observed to rise significantly. These conditions are significant public health concerns, given their potential to progress unnoticed in the absence of symptoms until advanced stages. Health systems across the globe are now facing an escalating challenge in managing the consequences of NAFLD. This rise emphasizes the importance of increasing awareness and education surrounding these conditions, both for the public and healthcare practitioners, to ensure early identification and intervention.
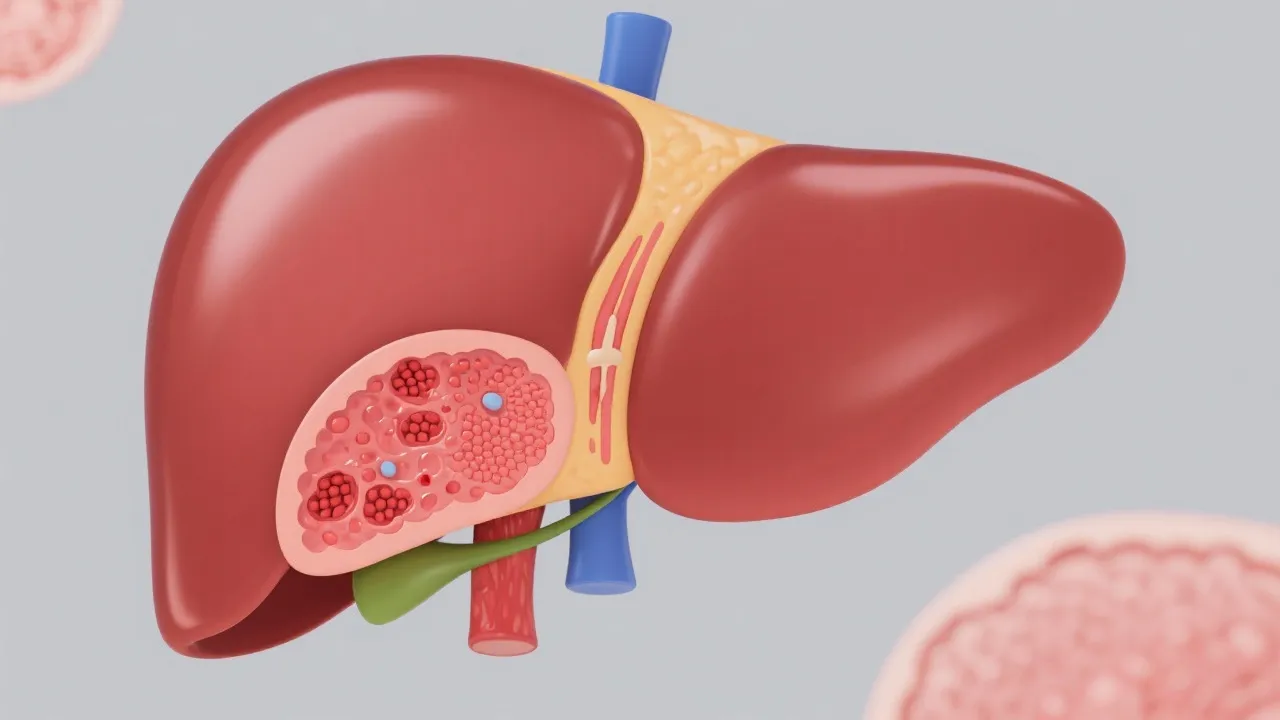
The pathogenesis of NAFLD related HCC is complex and multifactorial. NAFLD encompasses a spectrum of liver conditions, ranging from simple steatosis to non-alcoholic steatohepatitis (NASH), which carries the potential to develop into cirrhosis, thereby increasing the risk of HCC. The accumulation of fat in liver cells can lead to cell injury, mitochondrial dysfunction, and chronic inflammation, creating a conducive environment for cancerous changes. In more detail, the progression often initiates with simple fat accumulation (steatosis), which may not cause significant damage but can lead to cellular stress. When inflammation sets in, as seen in NASH, the situation deteriorates. Inflammatory mediators and cytokines can cause further damage to hepatocytes, and the resultant fibrosis can eventually progress to cirrhosis — a crucial risk factor for HCC.
In addition to inflammation and fibrosis, oxidative stress plays an integral role in the disease pathway. The liver's exposure to excess free fatty acids results in an overproduction of reactive oxygen species (ROS). These ROS can lead to lipid peroxidation, DNA damage, and ultimately, mutagenesis. Genetic and epigenetic changes may occur, leading to oncogenic transformation of liver cells, thus enhancing the risk of HCC as the disease advances. Another important aspect to consider is the interplay of insulin resistance — often stemming from obesity and sedentary lifestyles — further aggravating the fatty liver condition and increasing the risk of hepatic oncogenesis. Emerging research also highlights interesting interactions between the gut microbiome and liver disease, implicating dysbiosis as a potential contributor to NAFLD progression.
Several risk factors can heighten the risk of NAFLD progressing to HCC. These include obesity, insulin resistance, type 2 diabetes, and genetic predispositions. Moreover, dietary patterns, physical inactivity, and age play a significant role in exacerbating these risks. Each of these factors contributes uniquely to the pathophysiological state that leads to advanced liver disease and presents complex challenges to health outcomes. Obesity is perhaps the most significant risk factor, closely linked to metabolic syndrome, which encompasses a constellation of conditions including hypertension and dyslipidemia, ultimately leading to NAFLD and potential liver cancer.
Insulin resistance serves as a crucial mechanism in this condition, promoting lipogenesis and reducing fatty acid oxidation, thereby leading to steatosis. Those with type 2 diabetes are particularly at risk; research suggests that the prevalence of NAFLD is significantly higher in diabetic patients compared to the general population. Furthermore, age is a critical risk factor, as older adults naturally have increased prevalence and severity of hepatic fibrosis, exacerbating the risk of HCC due to prolonged duration of liver disease. Notably, genetic predispositions can further complicate these risks. Certain ethnic groups, particularly those of Asian ancestry, may be genetically predisposed to more aggressive forms of NAFLD and HCC, necessitating tailored screening guidelines and preventive measures. Additionally, lifestyle choices, such as high-calorie diets rich in fructose or trans fats, have been recognized as contributors to NAFLD's progression.
Timely diagnosis is vital for effective management and improved outcomes of NAFLD related HCC. Ultrasound imaging, CT scans, MRI, and liver biopsies form the cornerstone of current diagnostic practices. Ultrasound is often first-line due to its non-invasive nature and cost-effectiveness. However, it may have limitations in specificity, especially in distinguishing simple steatosis from advanced liver disease. CT scans provide more detailed imaging, allowing better assessment of liver anatomy, fat content, and the detection of lesions that may suggest HCC. MRI, particularly with liver-specific contrast agents, has emerged as a powerful tool, offering excellent soft-tissue contrast and aiding in the differentiation of benign from malignant lesions.
Blood tests measuring liver function and biomarkers like alpha-fetoprotein (AFP) aid in identifying at-risk individuals. Although elevated levels of AFP are associated with HCC, its specificity is not absolute; hence, there is an urgent need for more precise and less invasive diagnostic tools. Advanced imaging modalities like elastography can non-invasively measure liver stiffness, reflecting the degree of fibrosis, and assist in risk stratification. Some researchers are exploring the potential use of artificial intelligence (AI) in imaging interpretation to enhance detection rates of early liver malignancy. Furthermore, emerging biomarkers such as cytokeratin 18 fragments and microRNAs are being studied extensively for their possible roles in early diagnosis, offering promising avenues for the future of diagnostic strategies.
Management of NAFLD related HCC requires a multidisciplinary approach, encompassing lifestyle changes, pharmacological interventions, and surgical options. Weight loss and exercise play a crucial role in reducing the liver's fat content and alleviating inflammation. Even modest weight reduction (as little as 5-10% of body weight) has been shown to significantly improve liver histology and metabolic parameters in individuals with NAFLD. Exercise, including both aerobic and resistance training, further complements dietary interventions, providing beneficial effects on insulin sensitivity and hepatic fat content.
Pharmacological treatments, like insulin-sensitizers (such as metformin) and lipotoxicity reducers (including medications like omega-3 fatty acids), offer potential benefits in managing NAFLD. Other emerging drugs target pathways involved in liver inflammation and fibrosis, such as GLP-1 receptor agonists, which have also demonstrated weight loss benefits. In advanced cases, options include surgical resection, liver transplantation, and radiofrequency ablation, although availability and effectiveness may vary based on the patient's overall health and the extent of liver disease. It is crucial for healthcare providers to engage patients in shared decision-making to tailor medical and surgical interventions, ensuring personalized care plans that account for individual risks and preferences. Supportive care, including nutritional counseling and mental health support, should also be integrated into the management of these patients to enhance adherence to lifestyle changes and improve overall quality of life.
Prevention of NAFLD related HCC hinges on mitigating modifiable risk factors. Public health initiatives advocating for healthier lifestyles, dietary adjustments, and physical activity could counter the upward trend of NAFLD. Comprehensive awareness campaigns that exemplify success stories can inspire individuals to take positive actions regarding their health. Additionally, implementing community-based programs that provide education, support, and resources for weight management and balanced eating can significantly impact public health outcomes.
Moreover, as research progresses, new therapeutic targets and potential vaccines offer hope for reducing the burden of this condition. Ongoing studies exploring the role of gut microbiota and its interaction with liver health may reveal novel therapeutic strategies to modulate disease progression. Collaborative efforts between healthcare providers, policy-makers, and researchers are essential in paving the way forward. Implementation of routine screening for at-risk populations, particularly those with diabetes and obesity, can facilitate early detection of liver disease before it advances to a more severe stage.
In addition, addressing the social determinants of health, such as access to nutritious food, healthcare services, and opportunities for physical activity, are paramount in creating an environment that encourages a healthy lifestyle. The emphasis should shift towards a preventative health model, where the focus is on maintaining metabolic health and liver function to minimize the overall incidence of NAFLD and its resultant complications, including HCC. Embracing technological advancements in telemedicine can also enhance patient monitoring and provide more personalized approaches to managing risk factors remotely.
Case studies and real-world success stories can offer valuable insights into effectively managing NAFLD related HCC. Exploring such examples wherein individuals successfully reversed fatty liver disease through consistent lifestyle changes can inspire broader preventive health measures. For instance, one clinical case demonstrated how a 52-year-old male patient with a diagnosis of NASH experienced significant improvements in liver function through a structured weight-loss program combined with supervised exercise, leading to a reversal of some fibrosis markers. Another example may involve a woman who managed her diabetes and weight through a balanced diet rich in omega-3s and low glycemic index foods, resulting in her NAFLD improving significantly over 12 months.
Documenting medical advancements and clinical trial outcomes also enhance the body of knowledge, leading to improved standards of care. Successful implementation of lifestyle interventions can also be corroborated by studies indicating that programs focusing on diet and exercise led to a marked reduction in liver enzyme levels and improved quality of life `in` many participants. Documented success helps underscore the effectiveness of non-pharmacological strategies on liver health. Continuing to foster an environment for sharing these stories among individuals, healthcare professionals, and communities will empower others to proactively engage in their health with realistic and achievable goals. The integration of these case studies into educational materials can effectively highlight both the challenges and triumphs faced by those managing NAFLD, serving to motivate those at risk to seek help and commit to lifestyle changes.
| Risk Factor | Prevention Strategy |
|---|---|
| Obesity | Implement regular exercise routines and maintain a balanced diet, including whole grains and healthy fats. |
| Type 2 Diabetes | Manage blood sugar through appropriate medication, regular monitoring of glycemic control, and lifestyle modification. |
| Genetic Predisposition | Regular screening and early lifestyle intervention for at-risk individuals; consider genetic counseling. |
| Poor Dietary Choices | Avoid processed foods high in sugars and trans fats; increase intake of fruits, vegetables, and lean proteins. |
| Lack of Physical Activity | Engage in at least 150 minutes of moderate-intensity aerobic exercise per week; integrate strength training twice a week. |
| Age | Regular check-ups and screenings should be prioritized, especially for individuals over 40. |
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
