Non-Alcoholic Fatty Liver Disease (NAFLD) and its progression to Hepatocellular Carcinoma (HCC) pose significant health challenges worldwide. This article explores the relationship between NAFLD and HCC, providing an objective analysis of the risk factors and potential preventive measures for individuals suffering from fatty liver disease.
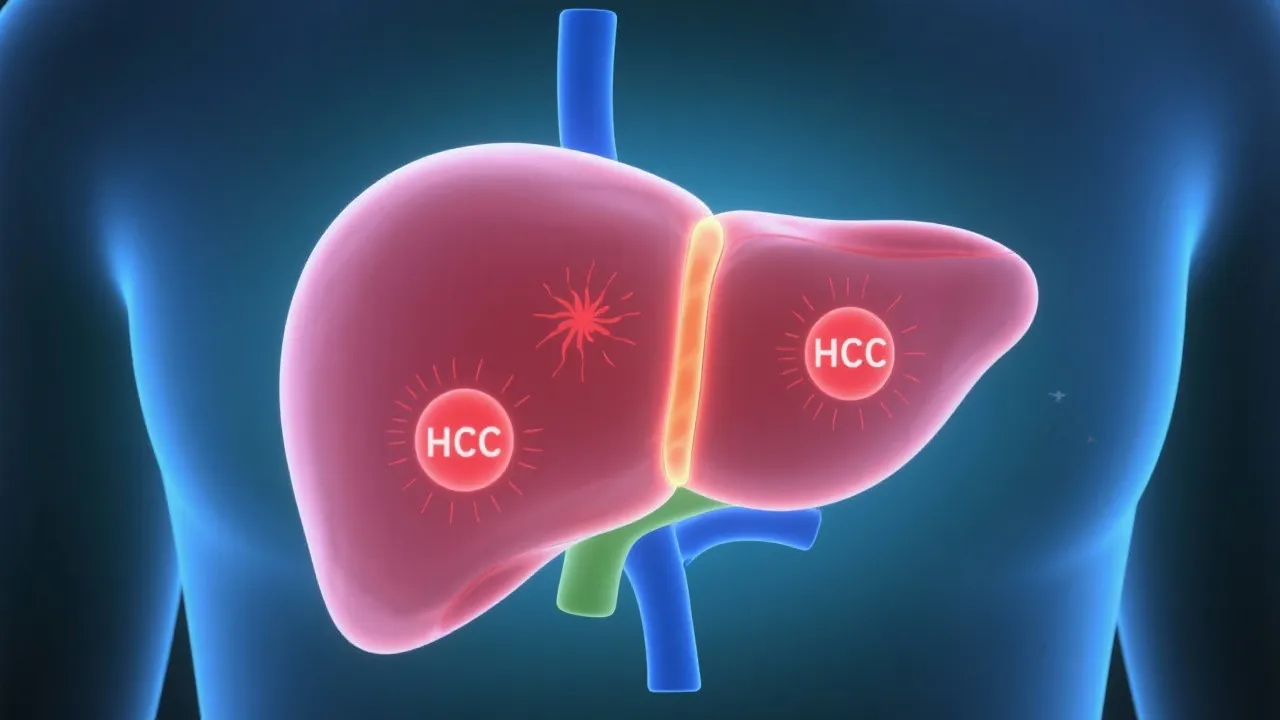
Non-Alcoholic Fatty Liver Disease (NAFLD) is increasingly recognized as a major public health issue. With its prevalence growing, an understanding of its potential progression to Hepatocellular Carcinoma (HCC) is crucial for effective management and prevention strategies. NAFLD encompasses a spectrum of liver conditions ranging from simple steatosis to non-alcoholic steatohepatitis (NASH), which can eventually lead to cirrhosis and HCC. The rising incidence of NAFLD and its complications underscores the need for comprehensive research and targeted interventions.
Research indicates that NAFLD is the most common chronic liver disease worldwide, affecting nearly 25% of the adult population globally. The condition is closely associated with metabolic syndrome, which includes obesity, hypertension, dyslipidemia, and insulin resistance. As NAFLD progresses, the liver becomes increasingly damaged by inflammation and fibrosis, setting the stage for more severe liver complications, including cirrhosis and HCC. With an aging population and rising obesity rates, the burden of NAFLD and its potential to cause liver cancer is expected to increase significantly over the coming years.
NAFLD-related HCC has become a focal point for researchers and healthcare professionals alike. The link between NAFLD and HCC lies in the gradual liver damage induced by fat accumulation, inflammation, and fibrosis. The liver can tolerate fat accumulation for some time; however, the transformation into NASH represents a critical point when inflammation and damage ensue. Unlike alcoholic liver disease, NAFLD progresses without the influence of alcohol, making lifestyle choices, dietary habits, and genetic factors significant contributors to disease onset and progression.
In recent years, studies have shown that the presence of hepatic steatosis itself is a strong predictor of liver-related morbidity. As steatosis progresses to NASH, the risk of cirrhosis increases considerably. Once cirrhosis develops, there is a significantly heightened risk of HCC. It is estimated that 5% to 15% of patients with NASH may progress to cirrhosis, and approximately 5% to 10% of those with cirrhosis will develop HCC. This progression is concerning, highlighting the need for early detection and intervention strategies to stem this tide.
Identifying risk factors is vital in addressing NAFLD-related HCC. Key contributors include obesity, Type 2 diabetes, and dyslipidemia. Each of these factors plays a role in insulin resistance, which exacerbates hepatic fat accumulation and inflammation. The interplay between metabolic diseases and liver health demonstrates the complex nature of NAFLD progression. Additionally, lifestyle factors such as diet and physical inactivity further compound the risk, creating an environment ripe for disease progression.
Genetic predisposition and advanced age also play a significant role in disease progression. Genetic variants, such as those in the patatin-like phospholipase domain-containing protein 3 (PNPLA3) gene, have been implicated in increased susceptibility to liver fat accumulation and inflammation. Furthermore, gender differences have been noted, with males generally at a higher risk than females. This disparity is thought to stem from hormonal differences and variations in fat distribution, impacting liver metabolism and inflammation differently between genders.
Moreover, certain comorbid conditions, such as hypertension and obstructive sleep apnea, have also been associated with an increased risk of NAFLD and its progression to HCC. Obesity leads to adipose tissue dysfunction, which in turn promotes systemic inflammation. This chronic, low-grade inflammation contributes further to liver damage, fibrosis, and the eventual transformation into cancerous cells. The cumulative impact of these risk factors necessitates a critical and proactive approach to prevention and management.
Preventive measures focus on lifestyle modifications, emphasizing weight management, regular physical activity, and a balanced diet rich in nutrients. These lifestyle changes are paramount in mitigating the risk of NAFLD progression and its complications. Studies have suggested that even modest weight loss (5-10% of body weight) can lead to significant improvements in liver histology and function. Regular physical activity, defined as at least 150 minutes of moderate aerobic exercise per week, has been shown to improve insulin sensitivity and promote weight loss, hence positively affecting liver health.
Nutrition plays a crucial role, especially adopting dietary patterns such as the Mediterranean diet, which is known for its beneficial effects on metabolic health. This diet emphasizes whole grains, healthy fats from sources like olives and nuts, lean proteins, and abundant fruits and vegetables. Additionally, limiting refined sugars and processed foods is essential in managing NAFLD. Recent studies have indicated that reducing sugar intake, particularly fructose, can be particularly effective in curbing liver fat accumulation.
Early detection through surveillance and regular liver function testing is essential in managing high-risk individuals. For those diagnosed with NAFLD, a comprehensive assessment that includes imaging studies and possibly liver biopsy may be warranted to ascertain the severity of the condition. Interventions may include medical therapies such as the use of insulin sensitizers (like metformin) and lipid-lowering agents (like statins), which show promise in mitigating NAFLD progression. Additionally, vitamin E supplementation has been considered for certain patients with NASH, particularly if they do not have diabetes.
NAFLD-related HCC diagnosis relies on imaging techniques, such as ultrasound, CT, and MRI, alongside biomarker assessments. Regular surveillance for populations at risk is integral, with emerging non-invasive biomarkers offering potential for early detection. Imaging studies play a crucial role in detecting liver tumors, and new technologies are continually being developed to enhance detection rates. For instance, contrast-enhanced ultrasound and advanced MRI techniques have shown promise in improving diagnostic accuracy.
Continuous monitoring enables timely intervention, reducing the risk of cancer development. Individuals with cirrhosis due to NAFLD are generally recommended to undergo regular surveillance with ultrasound every six months, along with consideration for serum alpha-fetoprotein (AFP) testing. The use of serum biomarkers, such as the LFS (Liver Failure Score) and Fibrosis-4 index (FIB-4), can assist in stratifying patient risk and tailoring surveillance strategies effectively.
Challenges remain, particularly in distinguishing between benign liver lesions and early-stage HCC. Advances in liquid biopsy technologies are exciting prospects in this arena, with studies indicating the potential for circulating tumor DNA to aid in early detection and monitoring of HCC progression. These developments underscore the importance of personalized approaches to diagnosis and management based on individual patient profiles.
| Management Approach | Description |
|---|---|
| Lifestyle Modifications | Encourages weight loss, physical activity, and dietary adjustments to reduce liver fat. Evidence suggests that even a slight reduction in weight can yield significant hepatic benefits. |
| Pharmacotherapy | Involves using medications like metformin and statins to improve liver health and metabolic parameters. Ongoing research aims to identify additional therapeutic agents that can target the underlying mechanisms of liver injury. |
| Surveillance | Regular monitoring through imaging and biomarkers to detect early signs of HCC. Enhanced surveillance programs may significantly reduce mortality in high-risk populations. |
| Interventional Procedures | In cases of advanced liver disease or developed HCC, interventions such as radiofrequency ablation or liver transplantation may be necessary for patients with cirrhosis. |
Industry experts highlight the significant strides in understanding the NAFLD-HCC link, emphasizing the importance of integrated care approaches. Multidisciplinary teams involving dietitians, endocrinologists, hepatologists, and primary care providers are essential in the management of NAFLD to ensure comprehensive care. Research continues to explore novel therapeutic targets and preventive strategies, with an interdisciplinary focus on nutrition, pharmacology, and genetics.
In addition to the traditional management approaches, innovative interventions such as behavioral therapy aimed at promoting lifestyle changes have shown promise in clinical practice. As new data emerges, strategies might include the incorporation of telehealth for continuous patient engagement and education regarding proactive health management.
There is also growing interest in the role of gut microbiota in NAFLD and its relation to liver disease progression. Studies have indicated that alterations in the gut microbiome may contribute to the inflammation and metabolic dysfunction observed in NAFLD, making it an exciting area for future research and potential therapeutic interventions.
As we move forward, research efforts must focus on understanding the pathophysiology of NAFLD and its progression to HCC in finer detail. Longitudinal studies tracking metabolism, liver function, and genetic markers are vital in defining risk profiles and developing targeted therapies to intervene at critical points in disease progression. There is a pressing need for large-scale epidemiological studies that investigate the long-term outcomes of various treatment strategies in different populations across the globe.
Furthermore, exploring the role of personalized medicine—tailoring treatment based on individual genetic, phenotypic, and lifestyle-related factors—can significantly impact management outcomes. Potential treatments may include new pharmacological agents targeting the underlying pathways of steatosis, inflammation, and fibrosis that characterize NAFLD.
In conclusion, NAFLD-related HCC represents a significant healthcare challenge, necessitating a multi-faceted approach encompassing lifestyle changes, medical interventions, and continuous research into innovative treatments. Understanding and managing this link is crucial in reducing liver cancer incidence globally. With an aging population and increasing prevalence of obesity, urgent attention to NAFLD and its implications for public health policy is imperative. By prioritizing research and prevention strategies, we can work towards ameliorating the burden of liver disease and improving health outcomes for millions worldwide.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
