This article delves into the relationship between induced pluripotent stem cells (iPSCs) and non-alcoholic fatty liver disease (NAFLD). It explores how iPSCs contribute to understanding NAFLD pathogenesis, offering potential therapeutic insights. As stem cell technology advances, it may transform our approach to tackling liver-related ailments.
Induced pluripotent stem cells (iPSCs) are a groundbreaking advancement in modern medicine. These cells are adult cells reprogrammed to an embryonic stem cell-like state, allowing them to differentiate into a variety of cell types. The ability of iPSCs to become any type of cell makes them invaluable in regenerative medicine, disease modeling, and drug testing. Among the diseases being studied in conjunction with iPSCs is non-alcoholic fatty liver disease (NAFLD). This innovative technology has opened new avenues for understanding complex diseases and developing personalized medicine strategies.
The reprogramming of somatic cells into iPSCs was first achieved by Shinya Yamanaka and his team in 2006. This was a significant milestone in the field of cellular biology, as it provided a method to generate pluripotent cells from adult tissues, thus circumventing ethical issues associated with the use of embryonic stem cells. iPSCs retain the ability to self-renew and differentiate into multiple cell types, which makes them a powerful tool for both therapeutic and research applications. Their versatility is particularly notable, as they can be derived from a simple blood sample or skin biopsy, making them readily accessible for research and clinical applications.
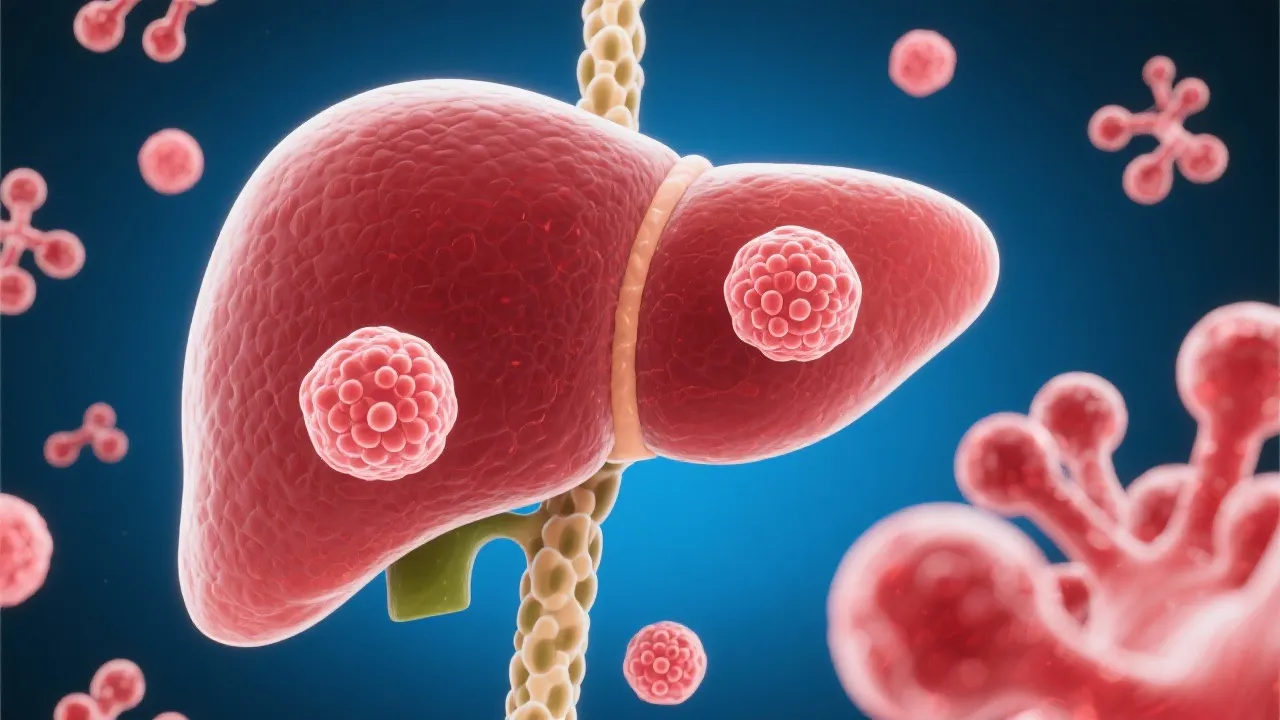
Non-alcoholic fatty liver disease is a spectrum of liver disorders ranging from simple steatosis (fat accumulation in liver cells) to nonalcoholic steatohepatitis (NASH), which can progress to liver cirrhosis and cancer. NAFLD is primarily associated with metabolic syndromes such as obesity and diabetes, affecting millions globally. The rising prevalence of this disease is alarming, particularly as obesity rates continue to climb worldwide. Recent studies estimate that NAFLD affects approximately 25% of adults globally, with figures indicating that the prevalence is markedly higher in specific populations, such as those with Type 2 diabetes and certain ethnic groups. Understanding its pathogenesis, preventative measures, and effective treatments is of paramount importance.
The pathophysiology of NAFLD is complex and multifactorial, involving genetic, environmental, and lifestyle factors. While the precise mechanisms leading to the development of NAFLD are not fully elucidated, insulin resistance has emerged as a pivotal factor in its pathogenesis. When insulin resistance occurs, the liver's ability to metabolize glucose and fatty acids is impaired, leading to the accumulation of lipids in hepatocytes and subsequent inflammation. Other contributing factors include oxidative stress, altered gut microbiota, and hormonal changes. As NAFLD progresses, it can lead to severe liver inflammation, fibrosis, and even hepatocellular carcinoma (liver cancer), highlighting the urgent need for effective therapeutic strategies.
Recent research highlights the potential of iPSCs to transform our understanding of NAFLD. By using iPSCs derived from patients with NAFLD, scientists can generate liver cells that reflect the individual's genetic makeup, allowing for a personalized approach to study disease progression. This capability is crucial for uncovering the cellular and molecular mechanisms underlying NAFLD. By utilizing patient-specific iPSCs, researchers hope to elucidate the heterogeneity of the disease, which varies significantly among individuals, and to identify potential biomarkers that can be used for early diagnosis and treatment monitoring.
Furthermore, iPSCs enable researchers to recreate the microenvironment of the liver in vitro, providing insights into the intricate interactions between liver cells, immune cells, and the extracellular matrix. Such models can mimic the fibrogenesis process seen in NAFLD and facilitate the discovery of new therapeutic strategies targeting specific pathways involved in liver inflammation and fibrosis.
The utilization of iPSCs provides an opportunity to screen for drugs and identify novel therapeutic targets. Given the complexity and variability of NAFLD, personalized treatments developed from patient-derived iPSCs could lead to more successful outcomes. Furthermore, these stem cells may contribute to regenerative therapies by replenishing damaged liver tissue. One of the most exciting prospects of using iPSCs in treating NAFLD is their potential to replace lost or damaged hepatocytes in patients who experience liver failure or advanced fibrosis.
Moreover, iPSCs can serve as a powerful platform for high-throughput drug screening assays. By differentiating iPSCs into hepatocyte-like cells, researchers can expose these cells to various pharmacological agents to evaluate their efficacy and toxicity. This is particularly beneficial for identifying compounds that can reverse the metabolic dysregulation observed in NAFLD. Additionally, the use of iPSCs can significantly reduce the reliance on animal models, which often do not accurately represent human disease due to differences in physiology.
Ongoing studies are investigating how iPSCs can be used to model NAFLD in vitro. Notably, researchers have succeeded in differentiating iPSCs into hepatocyte-like cells, effectively replicating aspects of liver function. These models offer critical insights into the fibrotic processes and lipid metabolism disturbances characteristic of NAFLD. Recent advancements include the incorporation of co-culture systems that involve other cell types, such as stellate cells and immune cells, to create a more sophisticated representation of the liver microenvironment.
In addition to modeling disease, researchers are exploring the genetic modification of iPSCs to express or knock out specific genes implicated in NAFLD. This gene editing potential provides a unique opportunity to study the role of specific proteins in disease progression and to identify new therapeutic targets. Technologies like CRISPR-Cas9 facilitate precise genome editing, allowing scientists to create relevant disease models that can mimic the genetic backgrounds of patients with NAFLD.
Moreover, the integration of bioinformatics and systems biology approaches is enhancing the understanding of NAFLD at a broader level. Computational models can analyze data derived from iPSC experiments, helping to identify genetic networks, signaling pathways, and metabolic alterations that contribute to the disease. As research continues to advance, high-dimensional data sets from single-cell sequencing and metabolomics will likely provide invaluable insights into the heterogeneity of NAFLD.
iPSCs are crucial because they allow for the derivation of patient-specific liver cells, providing a personalized platform to study NAFLD's progression and response to treatments. This method enhances our understanding of the disease's genetics and pathophysiology, leading to tailored therapeutic strategies based on individual patient profiles.
iPSCs are generated by introducing a set of transcription factors into adult cells, reprogramming them into a pluripotent state. This process makes them capable of differentiating into any cell type, including hepatocytes. The commonly used transcription factors for this conversion include Oct4, Sox2, Klf4, and c-Myc, often referred to as the Yamanaka factors.
While iPSCs alone cannot cure NAFLD, they play a significant role in developing new therapies and understanding the disease better. Their potential for regenerative medicine could contribute to future cures, as ongoing research explores the possibility of using iPSC-derived hepatocytes in cell replacement therapies. These applications are particularly promising in the context of advanced liver disease where existing treatment options are limited.
Since iPSCs are derived from adult cells, they do not carry the same ethical concerns as embryonic stem cells. However, issues regarding consent, the source of the cells, and potential commercialization of iPSC-derived therapies must be addressed to ensure ethical standards in research and clinical applications. Additionally, public perceptions surrounding stem cell research can influence funding and regulatory policies.
Advancements are needed in several areas, including improving the efficiency and safety of the reprogramming process, ensuring the stability of iPSCs during culture and differentiation, and enhancing techniques for scaling up production of specific cell types for therapeutic use. Furthermore, regulatory frameworks need to evolve to keep pace with the rapid developments in stem cell technologies to facilitate the translation of iPSC applications from the lab to the clinic.
While the potential of iPSCs in NAFLD research is vast, several challenges remain. The differentiation process is intricate, requiring precise conditions to ensure the accurate replication of liver-specific functions. Additionally, differences in patients' genetic backgrounds may lead to variations in differentiation efficiencies and functional outcomes, necessitating extensive optimization for each individual case. Quality control measures are essential to ensure that the generated hepatocyte-like cells consistently exhibit the desired characteristics.
There are also concerns about genetic instability and the possibility of tumor formation, emphasizing the need for stringent safety measures. Continuous monitoring of iPSC lines for chromosomal abnormalities and ensuring that any differentiated cells do not retain properties that could lead to oncogenesis are critical steps before clinical applications can proceed. Developers of iPSC-derived therapies must also address immunogenicity concerns to minimize the risk of immune rejection when these cells are transplanted into hosts.
Furthermore, the establishment of standardized protocols for iPSC generation and differentiation is essential. Collaborative efforts between academic researchers, regulatory agencies, and industry partners can help create consensus guidelines that enhance reproducibility and foster the development of safe and effective cell-based therapies.
Looking forward, advancements in iPSC technology, coupled with robust in vitro models and computational methods, will likely spur significant breakthroughs in NAFLD treatments. The use of bioengineered scaffolds combined with iPSC-derived cells offers promising approaches for reconstructing liver tissue in vitro, potentially allowing for organoids that can be used in drug testing or transplantation. Collaboration between stem cell researchers and clinicians is critical to translating these scientific discoveries into real-world therapies that could alter the landscape of liver disease management.
iPSCs represent a revolutionary tool in the fight against non-alcoholic fatty liver disease. Their application spans understanding disease mechanisms to pioneering novel treatments. The ability to generate patient-specific hepatocytes offers unprecedented opportunities for personalized medicine in addressing NAFLD. As research progresses, the integration of iPSCs in clinical settings promises to redefine liver disease diagnosis and management, bringing us closer to addressing a growing global health concern. Continuous investigation into the applications of iPSCs and the collaboration across scientific disciplines will be pivotal in shaping the future of treatments for liver diseases and beyond. By harnessing the power of iPSCs, we move towards an era where diseases like NAFLD can be managed with precision and ultimately cured.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
