This article explores the growing importance of non-alcoholic fatty liver disease (NAFLD) models in drug discovery. NAFLD, characterized by liver fat accumulation not caused by alcohol, is becoming a major health concern globally. Effective NAFLD models are crucial for understanding the disease mechanisms and developing therapeutic strategies. The article delves into the current advancements and future directions in this field.
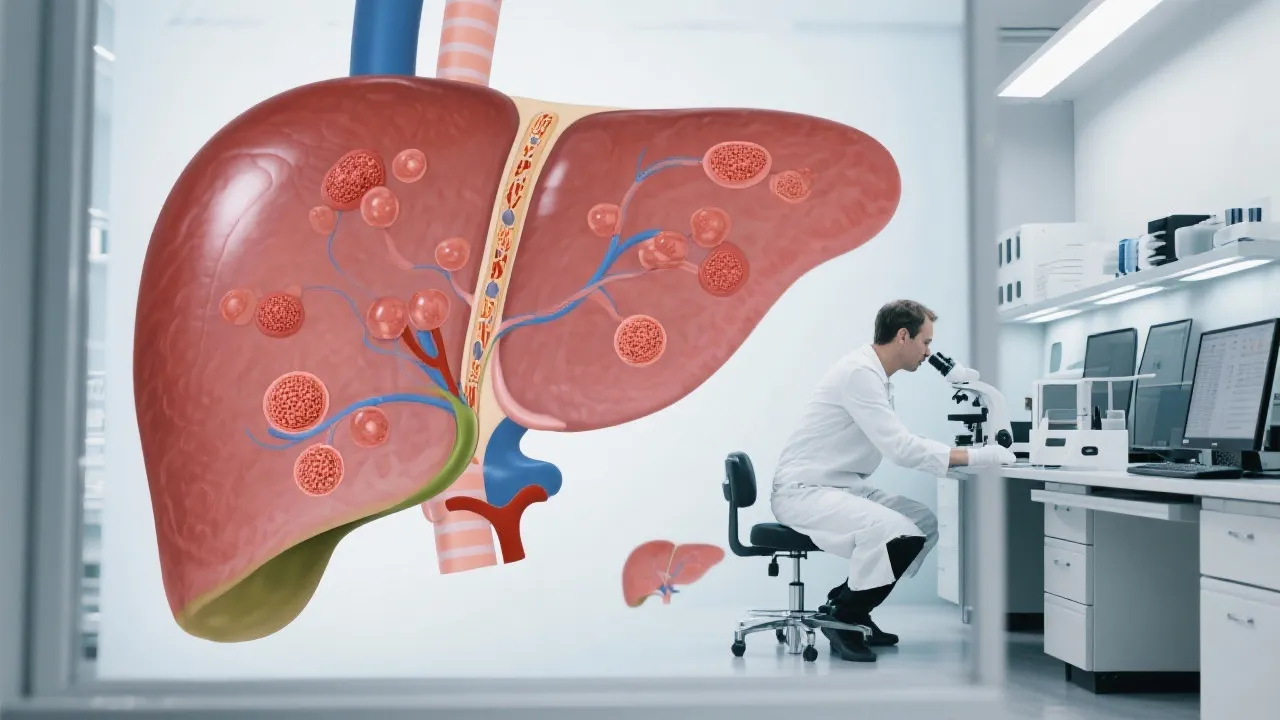
Non-alcoholic fatty liver disease (NAFLD) is increasingly becoming a focal point in the medical community due to its prevalence and potential for progression to more severe liver conditions. Unlike alcoholic liver disease, NAFLD occurs in individuals who consume little to no alcohol, making it a lifestyle-related disease closely tied to obesity, Type 2 diabetes, and metabolic syndrome. With society experiencing a rise in these conditions, the need for effective treatment options is paramount. Herein lies the importance of NAFLD models in drug discovery, providing a window into understanding disease mechanisms and honing therapeutic interventions.
Recent statistics indicate that NAFLD affects up to 25% of the global population, thereby attributing to it a significant burden on healthcare systems. The risk factors contributing to the development of NAFLD include sedentary lifestyles, high-calorie diets rich in carbohydrates and saturated fats, and genetic predisposition. As more individuals are diagnosed with NAFLD, it becomes essential to understand the spectrum of the disease, which can range from simple steatosis to non-alcoholic steatohepatitis (NASH) and eventually lead to cirrhosis and liver failure. Moreover, the connection between NAFLD and cardiovascular diseases has grown increasingly evident, highlighting the multifaceted impact of this condition on overall health.
NAFLD models are indispensable in the research and development of new therapeutic agents. These models are designed to replicate the human condition as closely as possible, offering a platform for testing the efficacy and safety of potential treatments before they advance to clinical trials. Effective NAFLD models embody the pathological features of the disease, including steatosis, inflammation, and fibrosis, allowing researchers to observe the drug’s impact on these critical clinical outcomes.
Utilizing accurate models helps to mitigate risks associated with drug development by providing insights into the pharmacological effects of medications under controlled conditions. This process is particularly important in the context of drug safety and effectiveness, which can vary significantly among different populations. For instance, how a drug behaves in a rodent model may differ greatly from its performance in human cells or tissues due to physiological variances. Thus, NAFLD models play a pivotal role not only in understanding disease mechanisms but also in ensuring that drugs are safe and effective before they are tested in clinical settings.
The evolution of NAFLD models reflects the broader strides being made in biomedical research. Traditional models, often involving rodent subjects, have expanded to incorporate more sophisticated systems, including genetically modified organisms, cell cultures, and organ-on-a-chip technology. Each model type presents unique advantages, with newly developed models offering insights that bridge gaps left by their predecessors. Notably, humanized liver models, which incorporate human cells into experimental setups, are on the rise, providing preventative insights into the pharmacokinetics and pharmacodynamics of drugs intended for human use.
One significant advancement in this area is the use of induced pluripotent stem cells (iPSCs), which can be derived from the patient’s own cells. This technology allows researchers to create liver organoids that closely mimic the patient’s liver function and response to treatment. The advantages of patient-specific models are manifold; they can reveal how a specific patient's genetic makeup influences NAFLD progression and drug response. This ability to personalize treatment approaches is paving the way for more effective therapeutic strategies, moving beyond one-size-fits-all models that may not account for individual variability in disease pathogenesis.
Moreover, advances in high-throughput screening methods allow for the evaluation of numerous potential therapeutic compounds in parallel, streamlining the drug discovery process. These innovative approaches not only save time but also reduce the overall costs associated with bringing new treatments to market. Enhanced computational methods and machine learning applications are also being integrated into the drug discovery process, allowing researchers to predict how changes in liver metabolism might influence drug efficacy and safety profiles.
Creating accurate and representative models of NAFLD is fraught with complications. One of the primary challenges lies in the complex etiology of the disease, which is influenced by a combination of genetic, environmental, and metabolic factors. Furthermore, translating findings from animal models to human conditions remains a significant hurdle due to physiological differences. As a result, researchers are increasingly focusing on human-based models, but these, too, bring challenges in terms of ethical considerations, scalability, and cost.
Additionally, while rodent models have been the standard in preclinical research for decades, recent findings suggest that their metabolic pathways differ significantly from those in humans, particularly in the context of lipogenic pathways. These discrepancies increase the difficulty in interpreting results from rodent studies, as the way a drug is metabolized and excreted can vary significantly between species. Such differences underscore the need for more sophisticated and representative human models.
Human liver cell lines present a promising alternative, yet they often lack the complexity observed in a normal liver environment, which contains a variety of cell types, including hepatocytes, stellate cells, and immune cells. The absence of cellular interactions could lead to a misrepresentation of drug responses and disease mechanisms. Similarly, while organ-on-a-chip technologies provide a microenvironment that simulates human tissue architecture and function, the field remains in its infancy, facing limitations in throughput and scalability that slow down research progress.
The future of NAFLD drug discovery is bright, buoyed by advancements in cutting-edge technologies such as CRISPR gene editing, artificial intelligence, and systems biology. These tools have the potential to revolutionize the development of NAFLD models by enhancing their precision and applicability. Moreover, embracing personalized medicine approaches can lead to models that account for individual variability in patient responses, ultimately tailoring therapies to patient-specific profiles.
CRISPR technology, for instance, enables precise genetic modifications that can be used to study specific genes associated with NAFLD, allowing researchers to delineate how variations in these genes contribute to disease susceptibility. This approach not only improves our understanding of the fundamental biology of NAFLD but also facilitates the identification of novel therapeutic targets that could be explored further in drug development pipelines.
Artificial intelligence (AI) is another promising tool. By analyzing vast datasets encompassing genetic information, clinical outcomes, and responses to treatments, AI can help identify patterns that may not be immediately apparent to human researchers. Such insights can lead to the development of more targeted therapeutics that are tailored to the unique genetic and environmental profiles of individuals. AI can also optimize the drug development process by predicting the efficacy and safety of new compounds early in the discovery phase, thereby reducing costly failures in later-stage clinical trials.
Systems biology approaches that integrate experimental data with computational modeling can also revolutionize how researchers understand the complexities of NAFLD. By simulating multiple biological processes simultaneously and assessing their interactions, systems biology can elucidate the multifactorial nature of NAFLD, revealing how different factors contribute to disease progression. In turn, these insights can guide drug development efforts towards agents that simultaneously target multiple pathways involved in NAFLD.
| Model Type | Advantages | Challenges |
|---|---|---|
| Rodent Models | Cost-effective, well-established protocols | Species differences, limited translatability |
| Cell Cultures | High control over environment, human cell use | Lack complexity of whole-organism systems |
| Organ-on-a-Chip | Mimics human physiology closely, microenvironment exploration | Technology still developing, limited throughput |
| Humanized Models | Incorporate human genetic and metabolic factors, personalized treatment potential | Ethical concerns, complexity in development |
| iPSCs | Patient-specific models, potential for drug screening and disease modeling | High cost and time of development, variability in differentiation |
The landscape of NAFLD research is evolving rapidly, underscoring the critical role of sophisticated models in drug discovery and therapeutic innovation. As our understanding deepens, so too does our capability to tailor therapies that meet the diverse needs of affected individuals, offering hope for effective management of this pervasive condition.
The importance of public awareness and education about NAFLD cannot be understated. Raising awareness about the disease can lead to earlier detection and intervention, improving patient outcomes. Public health initiatives aimed at promoting healthier lifestyles—such as improved nutrition, increased physical activity, and routine health screenings—are crucial in combating the rising prevalence of NAFLD. Encouraging communities to engage in preventative measures and fostering an environment that supports healthy living can potentially reduce the incidence of NAFLD significantly.
In conclusion, as the understanding of NAFLD and its implications expands, so does the potential for new therapeutic avenues. Researchers and clinicians must work collaboratively to bridge the gaps between scientific discovery and clinical application. By advancing NAFLD models and investing in innovative research methodologies, the medical community can unlock new possibilities for effective treatments and better patient care, ultimately addressing a condition that affects millions worldwide.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
