Non-alcoholic fatty liver disease (NAFLD) is gaining attention due to its increasing association with hepatocellular carcinoma (HCC), a primary form of liver cancer. This article explores the connection between NAFLD and the risk of HCC, outlining key factors, implications for health systems, and future research. Expert insights shed light on this growing medical concern and its impact on global health strategies.

Non-alcoholic fatty liver disease (NAFLD) has emerged as a significant public health concern due to its prevalence and potential progression to severe liver conditions such as hepatocellular carcinoma (HCC). As the liver accumulates excessive fat not attributed to alcohol use, NAFLD can advance to more severe forms, including non-alcoholic steatohepatitis (NASH), cirrhosis, and eventually HCC. The condition has gained attention due to its increasing incidence in the global population, with particular risks associated with obesity, metabolic syndrome, and sedentary lifestyles. Furthermore, public awareness about liver health and fat-related liver disease is critical as awareness leads to earlier diagnosis and potentially improved outcomes. NAFLD, which may initially appear benign, poses risks that make it fundamentally relevant in discussions about chronic diseases today.
Hepatocellular carcinoma primarily arises as a complication of chronic liver diseases, with NAFLD recognized as an important precursor. Increasing evidence substantiates that chronic liver conditions can set the stage for various complications, including advanced liver fibrosis and cirrhosis, which dramatically increase the risk of developing HCC. The rising incidence of NAFLD globally has simultaneously highlighted the increasing risk of developing HCC. This association underscores the necessity for medical professionals and researchers to focus on early detection, comprehensive monitoring, and innovative treatment options for individuals at risk.
Moreover, HCC is often diagnosed at advanced stages when treatment options are limited, highlighting a critical need for research into effective screening and biomarker development for those with NAFLD to prevent the potential progression to HCC. Continuous examination of the relationship between metabolic disturbances linked to NAFLD and cellular changes in the liver are pivotal factors in understanding and mitigating this risk.
Several factors contribute to the progression from NAFLD to HCC. These include genetic susceptibility, lifestyle factors such as diet and physical activity, comorbidities like obesity and type 2 diabetes, and environmental influences. Understanding these factors is crucial for developing targeted prevention and intervention strategies.
Genetic predispositions can manifest in various populations, suggesting that ethnogenetic factors play a role in susceptibility to liver diseases. Simultaneously, environmental factors such as exposure to toxins, dietary patterns rich in sugars and trans fats, and lack of physical activity are significant contributors to the increased body fat leading to NAFLD. Metabolic dysregulation stemming from obesity and insulin resistance is directly correlated with accelerated liver injury and the subsequent inflammatory response, which are key processes in disease progression.
Furthermore, hormonal influences connected with adipose tissue and leptin's role in inflammation are crucial. Advances in understanding these interconnected pathways not only enhance our understanding of NAFLD and HCC but also reveal potential intervention points for therapeutic approaches.
Recent studies have aimed at elucidating the biological mechanisms underlying the NAFLD-HCC progression. Efforts include identifying biomarkers for early detection, investigating genetic predispositions, and exploring novel therapeutic avenues that could hinder progression or reduce the associated morbidity and mortality. The identification of circulating microRNAs as potential biomarkers represents an exciting avenue for development, signaling liver inflammation and damage that may predict worsening disease. Other promising research avenues involve the use of imaging techniques that can non-invasively assess liver fat and fibrosis and technological innovations in genomics that allow for more personalized medicine approaches in treatment.
Moreover, clinical trials exploring the use of anti-inflammatory agents, such as pioglitazone and vitamin E, have shown promise in improving histological outcomes in patients with NASH. Future pharmacological treatments are also being investigated targeting pathways involved in fibrosis and cellular apoptosis that may present new strategies for preventing the progression from NAFLD to HCC. A multifaceted approach involving nutrition education, metformin for metabolic control, and weight reduction strategies can also help mitigate risks associated with NAFLD, ultimately lowering the incidence rate of HCC.
One of the primary challenges in managing NAFLD-related HCC is the asymptomatic nature of the early stages, which often results in delayed diagnosis and limited treatment options. Many individuals with NAFLD may be unaware of their condition as it often does not present noticeable symptoms until it has advanced significantly. Traditional risk factors do not always predict disease severity, complicating screening strategies. Surveillance programs and lifestyle interventions play a critical role in managing at-risk populations, underscoring the need for widespread public health initiatives.
Additionally, there is a pressing need for healthcare providers to emphasize patient education regarding liver health, fostering awareness around obesity, dietary patterns, and physical activity as preventative measures. Engaging patient communities through support groups and digital health platforms for tracking health metrics such as weight, liver enzyme levels, and lifestyle behavior can facilitate improved disease management. Furthermore, navigating the integration of lifestyle modifications into patient care plans requires a systemic approach involving multidisciplinary teams, including dietitians, mental health professionals, and primary care clinicians.
The burden of NAFLD and its complications, including HCC, poses a significant challenge to healthcare systems. The increasing prevalence demands enhanced resources for patient care, including advanced diagnostic facilities and specialized hepatology services. Policymakers must prioritize funding for liver disease research, making it a central focus of chronic disease management strategies. Expanded access to affordable obesity management programs, preventative health initiatives targeting at-risk populations, and the implementation of standardized screening protocols can help alleviate some of the healthcare burdens posed by NAFLD and HCC.
Moreover, increasing awareness and educational campaigns can arm practitioners with the knowledge necessary to identify those at risk and guide them toward effective intervention measures. Understanding and addressing social determinants of health, including access to nutritious foods and opportunities for physical activity, contribute to achieving better health outcomes for individuals affected by NAFLD.
Moving forward, research must focus on the multidimensional aspects of NAFLD-related HCC. This includes refining risk assessment models, enhancing early diagnostic tools, and developing integrative approaches that combine lifestyle interventions with pharmacological treatments. Expanding research efforts to assess the role of gut microbiota in modulating liver health can lead to innovative prevention and treatment strategies. Collaborative research initiatives that invite cross-disciplinary cooperation and global partnerships will be pivotal in advancing our understanding and management of this complex disease.
Finally, collaboration between academia, industry, and healthcare providers to fund and execute clinical trials exploring novel therapeutic agents will be essential. As researchers continue to explore various means of intervention, disseminating findings through open-access platforms could facilitate a broader application of effective strategies in diverse healthcare settings, ultimately benefiting those with NAFLD.
| Factor | NAFLD | HCC |
|---|---|---|
| Definition | Liver disease characterized by excess fat accumulation | Primary liver cancer stemming from liver disease |
| Risk Factors | Obesity, diabetes, sedentary lifestyle | Chronic liver disease, genetic predispositions |
| Complications | NASH, cirrhosis | Advanced liver disease, metastasis |
| Prevention Strategies | Lifestyle modifications, diet | Early detection, regular monitoring |
| Diagnosis | Often via imaging, liver biopsy | Primarily through imaging and histologic examination |
| Treatment | Weight loss, dietary change, pharmacotherapy | Surgery, ablation, systemic therapies |
| Prognosis | Generally favorable with lifestyle changes | Varies, generally worse if diagnosed late |
NAFLD affects approximately 25% of the global population, with varying prevalence rates across different regions influenced by lifestyle and genetic factors. In some regions, rates may peak as high as 40%. Furthermore, rising obesity rates associated with urbanization and dietary shifts play a significant role in the increasing cases reported.
In its early stages, NAFLD can be reversible through lifestyle changes, including diet, exercise, and management of comorbid conditions. Engaging in regular physical activity and ensuring a healthy diet rich in fruits, vegetables, whole grains, and lean proteins can significantly improve liver health, promote weight loss, and reverse fat accumulation in the liver.
The progression involves a series of liver damage stages, starting from steatosis to inflammation, fibrosis, and ultimately cirrhosis, creating an environment conducive to the development of HCC. Each stage represents a myriad of cellular and molecular changes that culminate in oncogenic transformations leading to cancerous growth.
Early symptoms may be nonspecific or absent. As HCC progresses, symptoms might include abdominal pain, weight loss, jaundice, and liver dysfunction. Late-stage symptoms often reflect the severity of liver impairment and may include abdominal swelling, confusion, and severe fatigue. Early intervention is crucial, since symptom onset often indicates advanced disease requiring immediate attention.
Preventing NAFLD typically involves adhering to a balanced diet rich in nutrients, maintaining a healthy weight, engaging in regular physical activity, avoiding excessive alcohol consumption, and managing comorbid conditions such as diabetes, hypertension, and dyslipidemia. Monitoring liver health through regular check-ups and lab tests, especially for those with risk factors, is also a critical preventive strategy.
The link between NAFLD and HCC represents a significant medical challenge with implications for public health and healthcare systems worldwide. As the incidence of NAFLD rises, understanding its connection to liver cancer is crucial for developing effective prevention and treatment strategies. Continued investment in research, enhanced community education on liver health, and health systems' readiness to address the NAFLD epidemic are essential steps in combating this growing health threat. Collaborative research and proactive healthcare policies will be essential in addressing this complex and evolving issue that threatens to exacerbate the burden of chronic diseases globally, calling for a concerted effort from all health sectors to influence change.
Explore the Tranquil Bliss of Idyllic Rural Retreats

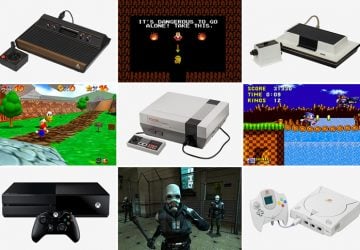
Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!
Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
