Non-alcoholic fatty liver disease (NAFLD) is an increasing health concern worldwide, leading to further complications such as hepatocellular carcinoma (HCC). This article delves into the connection between NAFLD and related HCC, discussing underlying mechanisms, risk factors, and potential preventive measures. It aims to provide an in-depth understanding of the disease progression and the latest research findings to enlighten healthcare professionals and the general public.
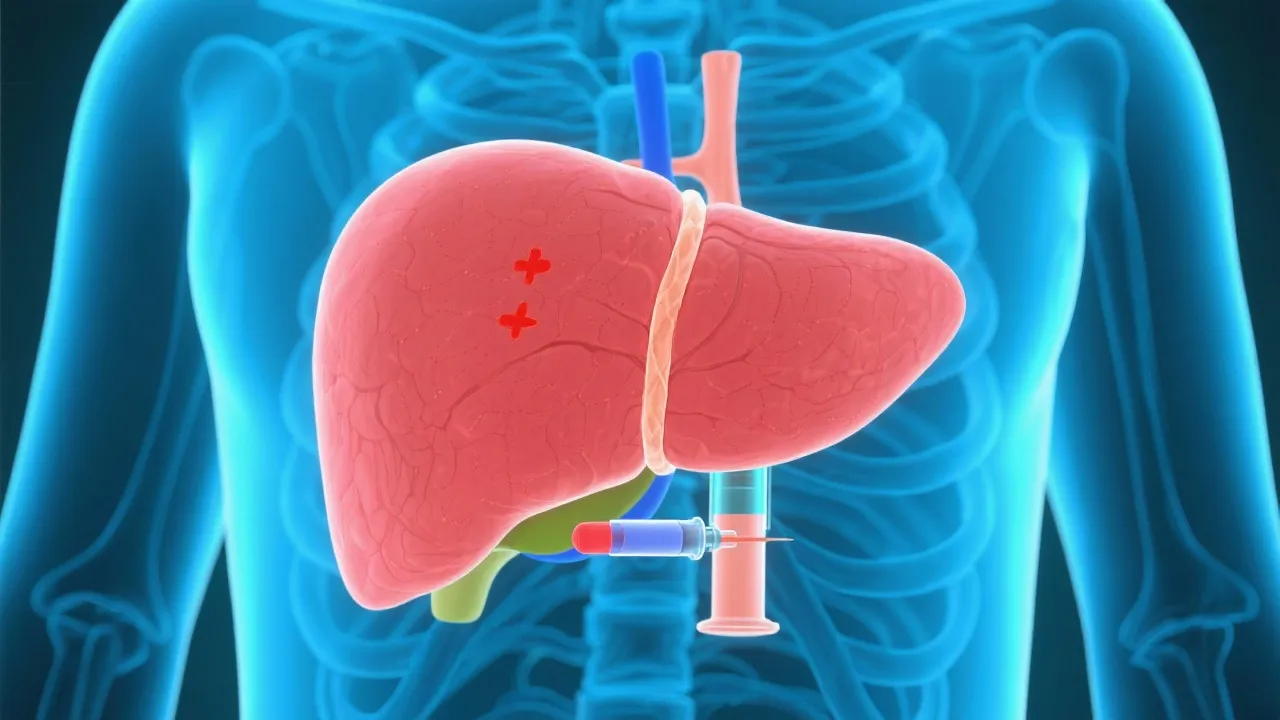
Non-alcoholic fatty liver disease (NAFLD) has emerged as a prevalent chronic liver condition globally. It is characterized by excessive fat accumulation in liver cells not caused by alcohol consumption. With lifestyle changes and the rising global obesity epidemic, NAFLD's prevalence has surged, affecting millions of individuals across various demographics. Recent studies have shown that NAFLD can progress into more severe liver conditions, including non-alcoholic steatohepatitis (NASH) and hepatocellular carcinoma (HCC). Recognizing the implications of this progressive liver disease is essential, as it not only impacts individual health but also places a significant burden on healthcare systems worldwide. Understanding the link between NAFLD and related HCC is critical for developing strategies to curb its growing epidemic.
NAFLD is increasingly recognized as a leading cause of HCC without cirrhosis. This form of cancer arises due to prolonged inflammation, fat accumulation, and liver cell damage. Medical experts emphasize that the liver's inflammatory response to fat deposition can trigger a cascade of events leading to fibrosis, necrosis, and ultimately the emergence of HCC. Notably, the progression from NAFLD to HCC often occurs in the context of metabolic syndromes like obesity, type 2 diabetes, and dyslipidemia.
Recent Research highlights the role of genetic factors and environmental influences in HCC development among NAFLD patients. Familial predispositions, exposure to environmental toxins, and the human microbiome all play a role in this pathway. The trajectory of disease progression underscores an urgency for early intervention and regular monitoring. In particular, the observation that a significant proportion of NASH patients can develop HCC prompts a reevaluation of how NAFLD is diagnosed and treated.
The transition from NAFLD to HCC involves complex biological mechanisms, including chronic inflammation, oxidative stress, and genetic mutations. Chronic inflammation in the liver typically accompanies fat accumulation and is triggered by the release of pro-inflammatory cytokines. These cytokines can recruit immune cells to the liver, exacerbating inflammation and setting the stage for fibrosis and cancerous changes. Hepatic stellate cell activation plays a pivotal role in liver fibrosis, advancing the risk of HCC. As these cells become activated, they transform into myofibroblast-like cells, contributing to collagen deposition and scarring in the liver.
Moreover, insulin resistance and hyperinsulinemia promote tumor growth by influencing cell proliferation and survival pathways. Insulin, through its signaling pathways, can enhance the survival of genetically altered cells within the liver, thereby increasing the risk of malignant transformation. A deeper understanding of these mechanisms is vital for identifying therapeutic targets to prevent HCC in NAFLD patients. Emerging research focuses on targeting specific molecular pathways implicated in this tumorigenesis process to halt or reverse the disease progression.
Several risk factors contribute to the transition from NAFLD to HCC. Comprehensive awareness of these factors can aid clinicians in identifying at-risk individuals who would benefit from increased surveillance and proactive measures. These include:
Effective strategies focusing on lifestyle modifications, pharmacotherapy, and surgical interventions are vital in preventing the progression from NAFLD to HCC. Understanding these multifaceted approaches allows healthcare providers to craft personalized treatment plans:
The field of NAFLD and HCC research is rapidly evolving, with numerous studies investigating the underlying mechanisms of disease progression, potential biomarkers for early detection, and novel therapeutic strategies. Emerging technologies, such as advanced imaging techniques and genomics, hold significant promise in improving our understanding of these complex conditions. Additionally, there is a growing interest in the microbiome's role in liver health. It is hypothesized that gut microbiota may influence metabolic health and the progression of liver diseases through mechanisms such as inflammation and fatty acid metabolism.
Future research initiatives should focus on identifying at-risk populations, improving diagnostic accuracy, and evaluating the long-term efficacy of both medical and surgical interventions. Collaborative efforts harnessing multidisciplinary perspectives will enhance our ability to tackle the growing burden of NAFLD and its progression to HCC effectively.
Q1: Can NAFLD lead directly to HCC?
Yes, NAFLD can lead to HCC without cirrhosis, although the exact mechanisms are still being studied extensively. The development of HCC in NAFLD patients often correlates with advanced liver inflammation and fibrosis.
Q2: What lifestyle changes can help prevent NAFLD-related HCC?
Adopting a healthy diet, engaging in regular physical activity, and avoiding excessive weight gain are recommended interventions. Regular health check-ups to monitor liver function and metabolic health are also essential.
Q3: Are there any genetic tests available to determine susceptibility to NAFLD-related HCC?
While some genetic predispositions have been identified, widespread and conclusive genetic testing for NAFLD-related HCC is not yet available. However, personalized medicine is an emerging frontier that aims to use genetic information to tailor prevention and treatment strategies.
Q4: How often should individuals with NAFLD be screened for HCC?
Patients with NAFLD should have their liver health monitored regularly, with many guidelines recommending biannual or annual screenings depending on the presence of risk factors such as age, diabetes, and the severity of liver disease. Early detection is critical in improving survival rates.
Q5: What role does diet play in managing NAFLD and preventing HCC?
Diet plays a pivotal role in managing NAFLD. Diets rich in healthy fats, lean proteins, and fiber while minimizing sugars and refined carbohydrates can significantly help in reducing liver fat and improving overall liver health. Dietary interventions should be individualized based on nutritional needs and preferences.
This article, grounded in current research, aims to provide a comprehensive understanding of the relationship between NAFLD and HCC. It stresses the importance of recognizing risk factors and implementing preventive measures to address the escalating burden of liver disease globally. Continued research and public health initiatives are necessary to mitigate the impact of NAFLD on individual health and broader societal implications.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
