This article delves into the innovative use of induced pluripotent stem cells (iPSCs) in researching Non-Alcoholic Fatty Liver Disease (NAFLD). iPSCs provide a dynamic tool for understanding liver diseases, marking significant progress in regenerative medicine. As researchers strive to uncover new therapeutic approaches, the synergy between iPSCs and NAFLD research could lead to revolutionary treatments and insights.
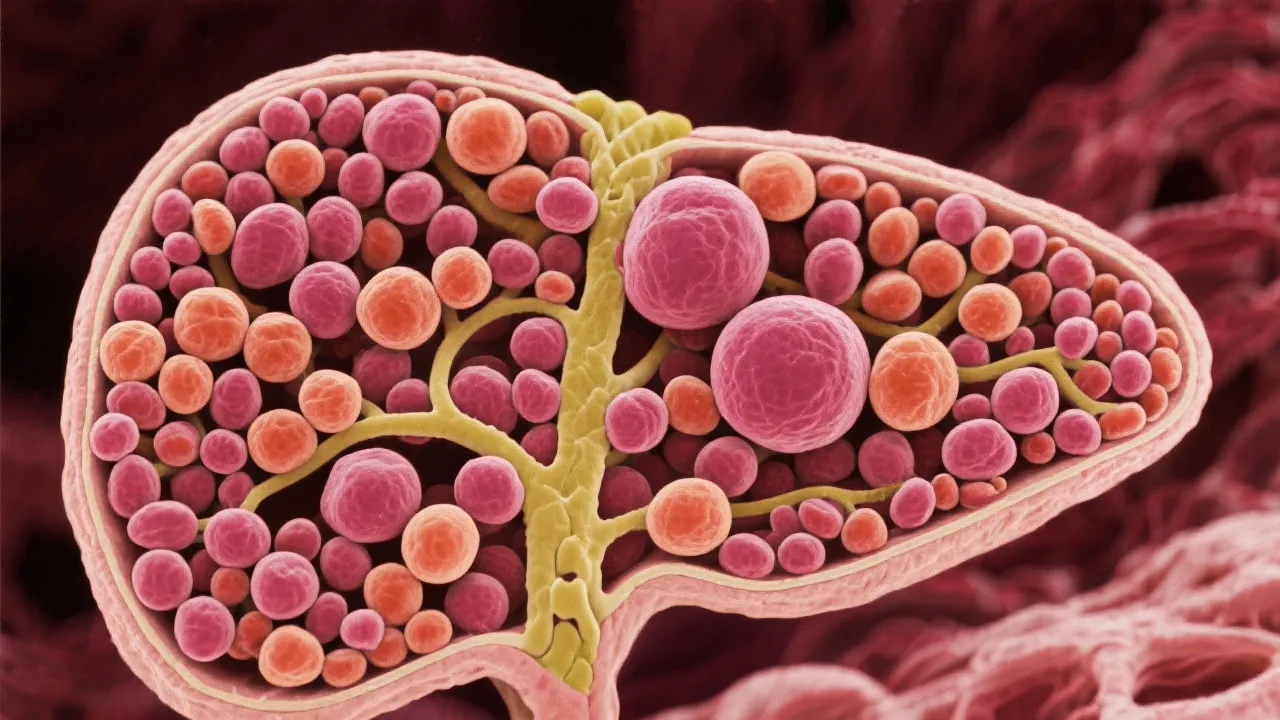
Induced pluripotent stem cells (iPSCs) are revolutionizing medical research by offering unprecedented insights into various diseases, including Non-Alcoholic Fatty Liver Disease (NAFLD). NAFLD is a complex liver condition characterized by excessive fat accumulation in the liver without significant alcohol consumption. Affecting a significant portion of the global population, it poses a challenge due to its potential to progress to more severe liver diseases, such as cirrhosis or liver cancer. The rise of NAFLD is paralleled by an increase in obesity and metabolic syndrome, which complicate its management and necessitate innovative research approaches. Understanding the underlying mechanisms of NAFLD through iPSCs can illuminate potential interventions that might ameliorate or halt disease progression.
iPSCs hold the promise of transforming research and therapy for NAFLD. By generating iPSCs from patients with NAFLD, researchers can create personalized liver cells in vitro. This provides a platform to study disease mechanisms at a cellular level, allowing for detailed investigation into genetic and environmental factors contributing to liver disease progression. The ability to generate liver cells from patients means that the interactions between specific genetic backgrounds and environmental triggers can be examined with a level of detail previously unattainable. For example, researchers can investigate how particular genetic mutations influence lipid metabolism and inflammatory pathways within the hepatocytes of individual patients.
Recent studies have highlighted the potential of iPSCs in modeling NAFLD. Through genetic analysis and drug screening, iPSC-derived liver cells offer insights into disease pathogenesis and therapeutic targets. For instance, researchers have used iPSC technology to observe how the human liver responds to certain fats or drugs, which can significantly differ from traditional animal models. Additionally, iPSC-derived hepatocytes can mimic the pathophysiological conditions of NAFLD, such as steatosis and steatohepatitis. Research indicates that iPSCs can be used to uncover novel biomarkers for early detection and to test new drugs effectively, advancing personalized medicine approaches in liver disease treatment. These breakthroughs are paving the way to identify new therapeutic avenues, enabling the possibility of tailored treatment strategies based on the molecular profile of the patient's liver cells.
Despite the promise of iPSC technology, certain challenges remain. Reproducibility and consistency of iPSC-derived cells pose ongoing concerns in research applications. Factors such as the source of the adult cells, the reprogramming method used, and the culture conditions can all lead to variability in the properties of the generated iPSCs and their differentiated derivatives. Furthermore, the transition from laboratory research to clinical application requires stringent validation processes to ensure safety and efficacy. For instance, ensuring that the differentiated hepatocytes truly replicate the function and pathology of native liver cells in humans requires extensive testing.
Moreover, ethical considerations surrounding stem cell research persist, although iPSCs mitigate some of these issues since they do not involve the destruction of embryos. However, issues related to genetic manipulation, consent, and the long-term implications of using such reprogrammed cells in therapies still need to be addressed comprehensively. Addressing these challenges together with regulatory harmonization could accelerate the development of novel treatments for NAFLD, improving patient outcomes significantly.
| Aspect | iPSCs | Traditional Research Methods |
|---|---|---|
| Cell Source | Patient-specific, reprogrammed adult cells | Animal models |
| Personalization | High potential for personalized medicine | Generalized to species, limited personalization |
| Scope for Discovery | Unlimited differentiation capability | Species-specific limitations |
| Pathophysiological Accuracy | Better mimicry of human disease conditions | Often do not replicate human disease accurately |
| Drug Testing | More relevant to human responses | May result in misleading results due to species differences |
Induced pluripotent stem cells (iPSCs) are a type of stem cell that can be generated directly from adult cells. They have the ability to differentiate into any cell type, offering vast potential in disease modeling and regenerative medicine. Unlike embryonic stem cells, iPSCs provide a relatively ethical and accessible option for developing therapies without significant ethical concerns related to embryo use.
iPSCs allow researchers to create patient-specific liver cells to study NAFLD's pathogenesis, test new therapeutic drugs, and explore potential genetic and environmental impacts on the disease. This cellular platform can be instrumental in elucidating mechanisms related to lipid metabolism defects, insulin resistance, and inflammation in the liver—hallmarks of NAFLD.
Challenges include ensuring the reproducibility and consistency of iPSC-derived cells, validating treatments in a controlled and rigorous manner before clinical application, and addressing ethical considerations surrounding the technology. Furthermore, the maturation of hepatocyte-like cells remains suboptimal, limiting the ability to study chronic liver diseases effectively.
There have been significant advancements in understanding disease mechanisms and identifying novel therapeutic targets, such as the involvement of specific signaling pathways in lipid accumulation. Additionally, iPSC models have successfully been employed to investigate the efficacy of various drug compounds in modulating disease progression, paving the way for future applications in personalized medicine.
The potential of iPSCs to cater to personalized medicine is particularly relevant for managing complex diseases like NAFLD. Future perspectives include the development of advanced biomaterials and 3D liver organoids derived from iPSCs that more accurately replicate the architecture and functionality of human liver tissue. These organoids can be utilized for high-throughput screening of drugs, enabling researchers to evaluate multiple compounds simultaneously, and fostering a rapid translation from bench to bedside.
Moreover, integrating iPSC-derived hepatocytes with artificial intelligence and machine learning can further accelerate drug discovery processes. By analyzing large datasets from patient-derived cells, researchers may discover unique patterns and predict responses to certain therapies, thus personalizing treatment plans for individuals based on their unique genotypes and disease phenotypes.
Institutions are also increasingly collaborating to establish biobanks of iPSC lines derived from diverse populations, ensuring representation and aiding in the discovery of new biomarkers for disease susceptibility. This collaborative effort can pave the way for globally applicable therapeutic strategies that address the variations in metabolic and genetic backgrounds that contribute to liver diseases across different demographics.
As the field of iPSC research expands, regulatory and ethical considerations play a crucial role in translating laboratory findings into clinical applications. Regulatory frameworks must adapt to the rapid advancements in technology to ensure the safe and effective use of iPSCs in therapies. This includes establishing guidelines for the manufacturing processes of iPSC-derived therapies, ensuring quality control and patient safety.
Ethically, researchers must consider issues related to patient consent for cellular reprogramming, the potential for genetic modifications, and how these interventions can affect future generations. A comprehensive ethical approach will include engaging with the public, policymakers, and ethicists to foster an open dialogue about the implications of using iPSCs in medicine, addressing concerns related to genetic privacy and equity in access to emerging therapies.
In conclusion, the integration of iPSCs in researching NAFLD presents a promising frontier in medical science. These cells provide a unique avenue for understanding the complexities of liver disease, advancing drug discovery, and offering personalized treatment options. As we continue to refine these technologies and overcome existing challenges, the potential for groundbreaking treatments in liver disease appears increasingly achievable. The future of NAFLD management may increasingly rely on tailored therapies that effectively target the pathophysiological nuances of individual patients, ultimately improving the prognosis and quality of life for those affected by this increasingly prevalent condition.
In addition to the promising avenues already discussed, several further research directions warrant exploration. One of the most compelling is the potential for gene editing technologies, such as CRISPR/Cas9, to enhance the therapeutic capabilities of iPSCs. By correcting genetic mutations at the stem cell level, researchers could potentially prevent NAFLD progression in genetically predisposed individuals. Additionally, this approach could enable the generation of iPSC lines that are more resilient to environmental insults, such as those caused by diet or toxins.
Another important area for advancement is the investigation of cellular reprogramming techniques. As scientists continue to refine methods for generating iPSCs, the efficiency and speed with which these cells can be derived can be vastly improved, resulting in more rapid clinical applications. Research should also focus on scaling up the production of iPSC-derived cells for therapeutic use while maintaining quality and functionality. Eventually, the establishment of standardized protocols can facilitate international collaborations and usher in a new era of precision medicine.
Integrating behavioral and lifestyle modification research with iPSC findings holds the potential to create multifaceted treatment plans for NAFLD patients. For instance, understanding how dietary changes or exercise might influence the cellular processes reflected in iPSC models could provide insights that translate into comprehensive lifestyle guidelines aimed at combating liver diseases.
Furthermore, collaborations between molecular biologists, hepatologists, and computational biologists may enhance the interdisciplinary approach required to unravel the multi-layered complexities of NAFLD. This will not only increase the throughput of research findings but also promote a deeper collective understanding of how to approach treatment from various angles, including molecular and environmental factors.
In summation, the future of iPSCs in liver disease research, particularly regarding NAFLD, is rich with possibilities. Building on current Momentum, the scientific community must push forward with determination and curiosity, seeking innovative solutions that may one day transform the landscape of liver disease treatment.
Explore the Tranquil Bliss of Idyllic Rural Retreats

Ultimate Countdown: The 20 Very Legendary Gaming Consoles Ever!

Understanding Halpin and its Influence

Affordable Full Mouth Dental Implants Near You

Discovering Springdale Estates

Illinois Dentatrust: Comprehensive Overview

Embark on Effortless Adventures: Unveiling the Top in Adventures Made Easy Outdoor Equipment

Unveiling Ossur Valves: Innovation in Prosthetics

Unlock the Full Potential of Your RAM 1500: Master the Art of Efficient Towing!
